SMALL BUSINESS
HEALTH
INSURANCE
EXCHANGES
Low Initial Enrollment
Likely due to Multiple,
Evolving Factors
Report to the Chairman, Committee on
Small Business, House of
Representatives
November 2014
GAO-15-58
United States Government Accountability Office

United States Government Accountability Office
Highlights of GAO-15-58, a report to the
Chairman, Committee on Small Business,
House of Representatives
November 2014
SMALL BUSINESS HEALTH INSURANCE
EXCHANGES
Low Initial Enrollment Likely due to Multiple, Evolving
Factors
Why GAO Did This Study
The Patient Protection and Affordable
Care Act required SHOPs—
exchanges, or marketplaces, where
small employers can shop for health
coverage for their employees—to be
established in all states. States may
elect to establish and operate SHOPs
themselves or allow CMS to do so
within the state. Enrollment in SHOPs
was to begin in October 2013, with
coverage effective as early as January
2014. GAO was asked to examine the
early implementation experiences of
the SHOPs.
In this report GAO describes (1) SHOP
functionality, enrollment, plan
availability, and premiums and
(2) stakeholders’ views on key factors
that have affected current SHOP
enrollment or may affect future
enrollment growth. GAO reviewed
relevant information from CMS and
states, including data on employer and
employee enrollment, plan availability,
and premiums generally through
June 1, 2014. GAO also interviewed
representatives of key stakeholders
that operate SHOPs (CMS and states),
offer coverage in SHOPs (health
insurance issuers), obtain coverage
through SHOPs (small employers), or
assist in obtaining coverage through
SHOPs (agents and brokers) on a
national basis and, for certain
stakeholders, in five states—California,
Illinois, Kentucky, Rhode Island, and
Texas. The five states were selected
based on factors including varied
issuer participation levels and SHOP
functionality. The experiences of these
stakeholders cannot be generalized to
other states or stakeholders.
GAO incorporated HHS comments on
a draft of this report as appropriate.
What GAO Found
Though all of the Small Business Health Options Programs (SHOPs) required by
the Patient Protection and Affordable Care Act were operational, many features
were not yet available and enrollment was low as of June 2014. According to the
Centers for Medicare & Medicaid Services (CMS), the agency that oversees the
SHOPs, all 33 of the SHOPs run by CMS (federally facilitated, or FF-SHOPs)
and 14 of the 18 SHOPs run by states (state-based, or SB-SHOPs) were
accepting enrollment applications as of the October 1, 2013, deadline. The
remaining 4 SB-SHOPs became operational by the following May. Websites
where employers could review plan information such as premiums and benefits
were available on October 1, 2013, for all FF-SHOPs and most SB-SHOPs.
Other key SHOP features—online enrollment and employee choice, the ability for
employees to choose among multiple plans—were delayed for all FF-SHOPs, but
available for most of the SB-SHOPs. CMS is currently preparing to implement
online enrollment for all FF-SHOPs and employee choice for many of the FF-
SHOPs for 2015. Based on official estimates and stakeholders’ expectations,
enrollment for the SB-SHOPs has been significantly lower than expected. The 18
SB-SHOPs had enrolled about 76,000 individuals—including employees, their
spouses, and dependent children—in plans purchased through nearly 12,000
small employers, as of June 1, 2014, for most states. Enrollment data for the FF-
SHOPs was not yet available, although CMS was in the process of collecting the
data from issuers and expected to have complete data by early 2015. However,
CMS officials said they do not expect major differences in enrollment trends for
2014 between SB-SHOPs and FF-SHOPs. Finally, most SHOPs had multiple
plans available in each county, although a small number of states had counties
with no plans available. Premiums for SHOP plans varied across states and were
generally comparable to premiums for other small group plans offered within a
state but outside of the SHOP.
Stakeholders identified several factors that may have led to current low SHOP
enrollment and that may affect future enrollment growth. Many stakeholders
reported that the primary incentive for employers to use the SHOPs has been the
small business tax credit available to eligible employers who offer coverage
through a SHOP, although some noted that the credit may be too small and
administratively complex to motivate many employers to enroll. Other factors
identified that may have hindered current enrollment include the ability of
employers to renew plans that existed before the SHOPs—which, depending on
state requirements, is permitted until October 1, 2016—and employer
misconceptions about SHOP availability. Stakeholders also described factors
that may help stimulate or detract from future SHOP enrollment growth. For
example, the phase-out of existing pre-SHOP plans, the implementation of
employee choice by an increasing number of SHOPs, improved coordination with
agents and brokers, and increased marketing to small employers may help
stimulate enrollment growth. Conversely, other factors, such as the 2-year limit
on the availability of the small business tax credit and the likelihood, according to
stakeholders, that SHOP premiums will not be lower than non-SHOP premiums,
may hinder future enrollment growth. The evolving and localized nature of these
factors suggests that that a determination of the SHOPs’ long-term impact
remains premature at this time.
View GAO-15-58. For more information,
contact John Dicken at (202) 512-7114 or
dickenj@gao.gov.
Page i GAO-15-58 Small Business Health Insurance Exchanges
Letter 1
Background 4
SHOPs Were Operational in All States, Although Many Expected
Features Were Not Yet Available and Enrollment Was Low as
of June 2014 9
Stakeholders Identified Several Factors That May Have Led to
Current Low SHOP Enrollment and That May Affect Future
Enrollment Growth 18
Concluding Observations 29
Agency Comments 29
Appendix I Small Business Health Options Program (SHOP) Features as of
June 1, 2014 31
Appendix II State-Based Small Business Health Options Program (SB-SHOP)
Enrollment Generally as of June 1, 2014 33
Appendix III Small Business Health Options Program (SHOP) 2014 Average
Monthly Premiums for Silver-Tier Plans 34
Appendix IV Small Business Health Options Program (SHOP) Silver-Tier Plan
Availability 36
Appendix V Comments from the Department of Health and Human Services 38
Appendix VI GAO Contact and Staff Acknowledgments 40
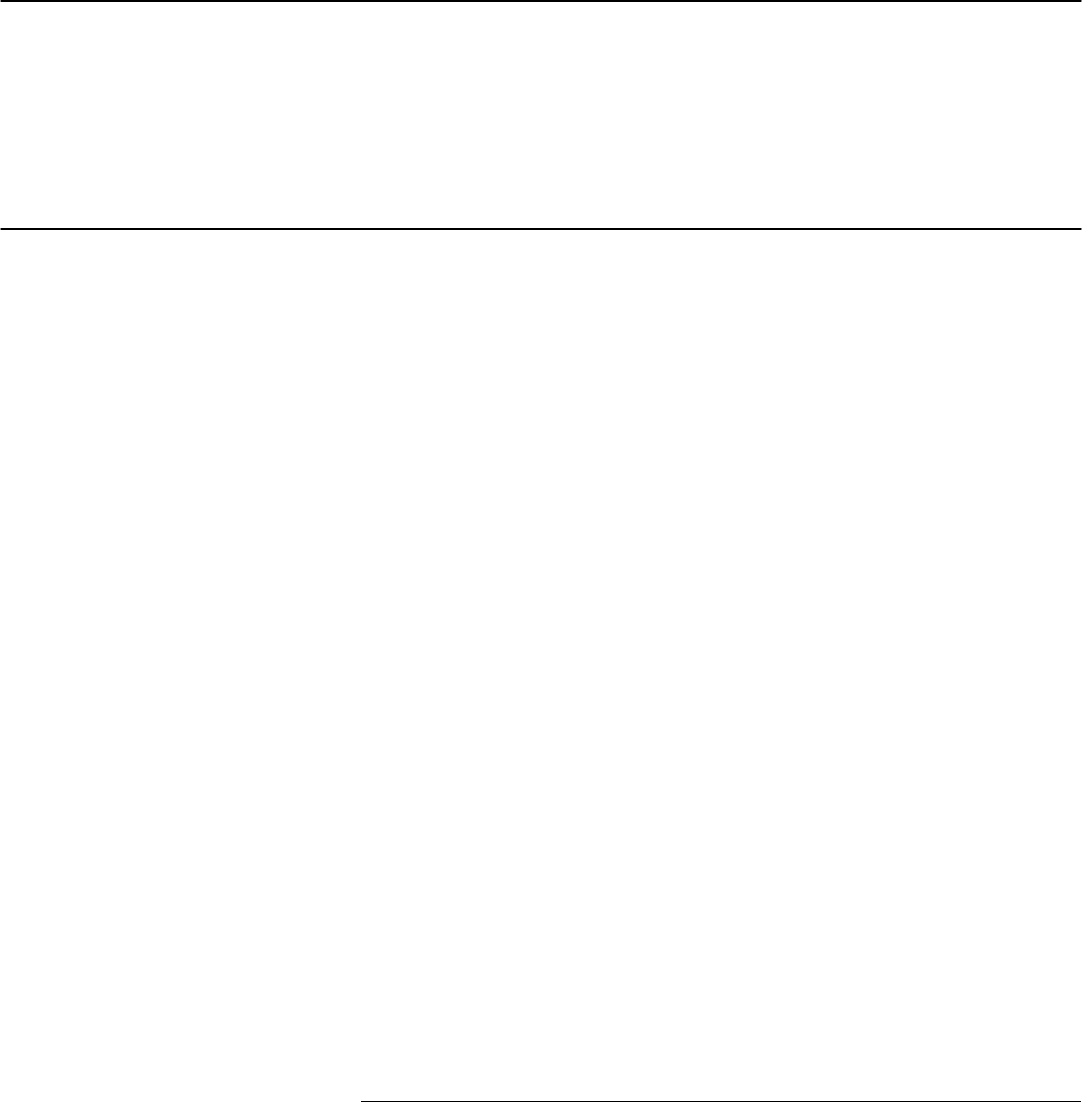
Figure
Figure 1: Total Enrollment in the State-Based Small Business
Health Options Programs (SB-SHOPs) Generally As of
June 1, 2014 13
Contents
Page ii GAO-15-58 Small Business Health Insurance Exchanges
Abbreviations
CBO Congressional Budget Office
CCIIO Center for Consumer Information and Insurance Oversight
CMS Centers for Medicare & Medicaid Services
FF-SHOP federally facilitated Small Business Health Options
Program
HHS Department of Health and Human Services
PPACA Patient Protection and Affordable Care Act
QHP qualified health plan
SB-SHOP state-based Small Business Health Options Program
SHOP Small Business Health Options Program
This is a work of the U.S. government and is not subject to copyright protection in the
United States. The published product may be reproduced and distributed in its entirety
without further permission from GAO. However, because this work may contain
copyrighted images or other material, permission from the copyright holder may be
necessary if you wish to reproduce this material separately.
Page 1 GAO-15-58 Small Business Health Insurance Exchanges
441 G St. N.W.
Washington, DC 20548
November 13, 2014
The Honorable Sam Graves
Chairman
Committee on Small Business
House of Representatives
Dear Mr. Chairman:
The Patient Protection and Affordable Care Act (PPACA) required the
creation in all states of Small Business Health Options Programs
(SHOPs)
1
—exchanges, or marketplaces, where small employers can
shop for and purchase health coverage for their employees.
2
SHOPs
were required to begin accepting enrollment applications for 2014
coverage by October 1, 2013, with coverage starting as early as
January 1, 2014.
3
A state may elect to establish and operate a SHOP
itself (through a state-based, or SB-SHOP) or allow the Department of
Health and Human Services’ (HHS) Centers for Medicare & Medicaid
Services (CMS) to establish and operate a federally facilitated SHOP
(FF-SHOP) within that state.
4
1
Pub. L. No. 111-148, §§ 1311(b), 1321(c),124 Stat. 119, 173, 186 (Mar. 23, 2010)
(codified at 42 U.S.C. §§ 18031(b), 18041(c)) (hereafter, “PPACA”), as amended by the
Health Care and Education Reconciliation Act of 2010, Pub. L. No. 111-152, 124 Stat.
1029 (Mar. 30, 2010) (hereafter, “HCERA”). In this report, references to PPACA include
any amendments made by HCERA.
In June 2013, we reported on the status of
federal and state efforts to establish the SHOPs. At that time, we found
that both CMS and states had made progress in establishing SHOPs,
In this report, the term “state” includes the District of Columbia.
2
PPACA also required the establishment of individual exchanges in each state where
eligible individuals can compare and select private insurance coverage from among
participating health insurance plans. The SHOPs and individual exchanges are intended
to provide single points of access to enroll employees of small businesses and individuals
into private health plans. Individual exchanges are also the access point to determine
eligibility for income-based premium subsidies and assess eligibility for other health
coverage programs such as Medicaid.
3
PPACA, § 1311(b)(1), 124 Stat. at 173 (codified at 42 U.S.C. § 13031(b)(1)); 45 C.F.R.
§ 155.410(b)-(c).
4
CMS has invited states to assist with certain FF-SHOP operations.
Page 2 GAO-15-58 Small Business Health Insurance Exchanges
although many activities remained to be completed and some were
behind schedule.
5
As the first year of SHOP operations nears its end, members of Congress
have raised questions about the challenges that SHOPs may face in
achieving long-term success. Such questions include whether SHOPs
have been able to provide online enrollment tools and other expected
functionalities, and in general whether SHOPs will offer sufficient value to
small employers to motivate them to enroll. You asked that we examine
the early implementation experiences of the SHOPs. In this report, we
describe
1. SHOP functionality, enrollment, plan availability, and premiums; and
2. stakeholders’ views on key factors that have affected current SHOP
enrollment or may affect future enrollment growth.
To describe early indicators of SHOP functionality, enrollment, plan
availability, and premiums, we requested information from CMS and
states and interviewed relevant officials. Specifically, to describe SHOP
functionality, including when SHOPs became operational, whether
SHOPs had a website that allowed employers to browse plan options and
enroll online, and whether SHOPs offered employers the ability to offer
their employees a choice among multiple plans, we requested information
from CMS and interviewed CMS officials. We analyzed CMS and SB-
SHOP data on plan availability and premiums in 2014, and we analyzed
SB-SHOP data on employer and employee enrollment for timeframes
ending between May and September 2014, with most ending on June 1,
2014. To assess the reliability of the data we received from CMS and
states, we performed manual and electronic tests of the data to identify
any outliers or anomalies and followed up with officials as necessary and
incorporated the corrections we received. We determined that the data
were sufficiently reliable for the purposes of our analysis. We also
reviewed other information sources, including published literature and
state SHOP websites, and identified federal requirements related to the
SHOPs by interviewing CMS officials and reviewing relevant laws and
regulations.
5
GAO, Patient Protection and Affordable Care Act: Status of Federal and State Efforts to
Establish Health Insurance Exchanges for Small Businesses, GAO-13-614 (Washington,
D.C.: June 19, 2013).
Page 3 GAO-15-58 Small Business Health Insurance Exchanges
To describe stakeholders’ views on key factors that have affected current
SHOP enrollment or may affect future enrollment growth, we interviewed
national-level representatives of key stakeholders that operate, offer
coverage in, obtain coverage through, or assist in obtaining coverage
through SHOPs. Specifically, we interviewed officials from CMS’s Center
for Consumer Information and Insurance Oversight (CCIIO) who oversee
the operation of SHOPs, as well as national organizations representing
issuers of health coverage, insurance commissioners, small employers,
and health insurance agents and brokers.
6
In addition, we selected five
states in which to interview state-level representatives of the SHOPs,
small employers, and agents and brokers.
7
To ensure that we captured a
range of SHOP-related experiences and perspectives, we selected states
that varied in terms of state population, geographic location, SHOP type
(FF-SHOP or SB-SHOP), SHOP website functionality, including the
availability of employee choice, and issuer participation in the SHOP. We
selected Kentucky, Rhode Island, California, Illinois, and Texas for our
study.
8
For the SB-SHOP states—Kentucky, Rhode Island, and
California—we interviewed state exchange officials. For the FF-SHOP
states—Texas and Illinois—we interviewed CMS officials involved with
the establishment and operation of the FF-SHOPs.
9
6
We interviewed representatives from the following national organizations: the Blue Cross
and Blue Shield Association, America’s Health Insurance Plans, the National Association
of Insurance Commissioners, the National Federation of Independent Business, and the
National Association of Health Underwriters.
Our work was limited
to reviewing illustrative examples of stakeholders’ experiences with and
perspectives on the SHOPs. The findings from our interviews therefore
cannot be generalized to the perspectives and experiences of all issuers,
insurance commissioners, employers, agents and brokers, or state
exchange officials.
7
The employer and agent and broker organizations for which we interviewed state-level
representatives were, respectively, the National Federation of Independent Business and
the National Association of Health Underwriters. We refer to state-level officials who have
participated in the establishment and operation of SHOPs as state exchange officials.
8
We interviewed agent and broker representatives in Kentucky, California, Illinois, and
Texas, and employer representatives in California, Rhode Island, and Illinois. The agent
and broker representative we contacted in Rhode Island and the employer representatives
we contacted in Kentucky and Texas elected not to participate in an interview.
9
We also interviewed state exchange officials in Illinois, who are assisting CMS in
operating the FF-SHOP in that state.
Page 4 GAO-15-58 Small Business Health Insurance Exchanges
We conducted this performance audit from February 2014 to November
2014 in accordance with generally accepted government auditing
standards. Those standards require that we plan and perform the audit to
obtain sufficient, appropriate evidence to provide a reasonable basis for
our findings and conclusions based on our audit objectives. We believe
that the evidence obtained provides a reasonable basis for our findings
and conclusions based on our audit objectives.
PPACA included a number of provisions that changed requirements for
small group health plans.
10
For example, PPACA required that, beginning
January 1, 2014, plans offer a set of minimum essential health benefits.
PPACA also set standards for the percentage of total average costs that
plans must cover for such benefits. The average costs covered by each
plan are reflected in different plan levels, or tiers, and each tier is
designated as bronze, silver, gold, or platinum.
11
In addition, beginning on
January 1, 2014, issuers are no longer able to consider the average
health status of a particular group when setting premium rates and can
only adjust premiums based on enrollment type (individual or family
enrollment), geographic area, age, and tobacco use.
12
PPACA required all small group health plans to comply with these
requirements as of January 1, 2014.
Plans meeting
these and other federal requirements, as well as other standards set by
states, may be certified to be offered in an exchange; these plans are
referred to as qualified health plans (QHPs).
13
10
These requirements apply to small group health plans whether they are sold inside or
outside of the SHOPs.
However, in response to concerns
regarding some issuers terminating plans that did not comply with PPACA
11
For a bronze-tier plan, on average, an employee would be responsible for 40 percent of
the costs of all covered benefits; for a silver-tier plan, on average, an employee would be
responsible for 30 percent; for a gold-tier plan, on average, an employee would be
responsible for 20 percent; and for a platinum-tier plan, on average, an employee would
be responsible for 10 percent of the costs of all covered benefits. PPACA requires that
issuers participating in an exchange offer, at a minimum, plans at both the silver and gold
levels of coverage.
12
There are further restrictions in the amount issuers can vary premiums based on the
ages and tobacco use of employees within a small group.
13
PPACA provided a narrow exception from these requirements for “grandfathered
plans”—health plans in which an individual was enrolled on March 23, 2010.
Background
Page 5 GAO-15-58 Small Business Health Insurance Exchanges
requirements, CMS announced in November 2013 that it would provide
transitional relief under which states could elect to permit issuers in their
states to offer renewals of their noncompliant plans for a plan year
beginning between January 1, 2014, and October 1, 2014, provided the
plans met certain conditions.
14
In March 2014, CMS extended this
transitional policy through October 1, 2016, and noted that the agency
may grant an additional 1 year extension, if necessary.
15
PPACA also mandated the establishment of SHOPs in each state to allow
small employers to compare available health insurance options in their
states and facilitate the enrollment of their employees in coverage. Until
2016, states have the option to define small employers either as
employers with 100 or fewer employees or employers with 50 or fewer
employees.
16
The SHOPs are required to have certain functionalities to facilitate the
health plan comparison and enrollment process. For example, each
SHOP must provide access to the SHOP to employers and employees
through a website, toll-free call centers, and in person. Each SHOP must
present the QHPs approved by the SHOP for the small-employer market
To be eligible for SHOP coverage, a small employer must
offer coverage to all full-time employees in a QHP through a SHOP. To
be eligible to enroll in a QHP through a SHOP, an individual must have
been offered health insurance coverage by a qualified employer through a
SHOP.
14
Conditions included that the coverage was in effect on October 1, 2013 and that
appropriate notices were provided to individuals and small employers. See Department of
Health and Human Services, Centers for Medicare & Medicaid Services, Centers for
Consumer Information & Insurance Oversight, Letter to Insurance Commissioners on
Market Transitional Policy, November 14, 2013, accessed September 8, 2014,
http://www.cms.gov/CCIIO/Resources/Letters/Downloads/commissioner-letter-11-14-
2013.PDF. According to CMS, 39 states adopted the transitional policy for 2014, while
12 states did not.
15
See Department of Health and Human Services, Centers for Medicare & Medicaid
Services, Extension of Transitional Policy through October 1, 2016, (Washington, D.C.:
Mar. 5, 2014). Under this policy, depending on state requirements, some small employers
may choose to remain enrolled in noncompliant plans through the end of plan years
beginning on or before October 1, 2016.
16
Under PPACA, beginning in 2016, small employers will be defined in all states as those
with 100 or fewer full-time equivalent employees. Beginning in 2017, states may allow
issuers of health insurance coverage in the large group market—issuers offering coverage
to groups of 101 or more full-time equivalent employees—to offer QHPs through the
SHOP and, in turn, will allow large employers to obtain coverage through the SHOP.
Page 6 GAO-15-58 Small Business Health Insurance Exchanges
in the state by the participating issuers of health coverage.
17
In addition,
the benefits, cost-sharing features, and premiums of each QHP must be
presented in a manner that facilitates comparison shopping of plans by
small employers and their employees. Each SHOP must accept employer
and employee applications through the SHOP website and may also
accept applications over the phone, in person, or by mail. This application
should collect the information necessary to screen an employer’s
eligibility for SHOP participation and identify employees eligible to enroll
in a QHP. Employers and employees may receive assistance to compare
coverage options and complete applications through a qualified insurance
agent or broker.
18
In addition, SHOPs will implement requirements related to employee
choice—that is, the ability of employees to choose a plan among multiple
plans offered to them by their employer.
19
17
All issuers or members of the same issuer group with a market share of greater than
20 percent in the state’s small group health insurance market must participate in a state’s
FF-SHOP if they wish to participate in its federally facilitated individual exchange. For
other issuers, participation is generally voluntary. States with SB-SHOPs may also impose
requirements related to issuer participation—for example, Maryland required issuers to
participate in its SB-SHOP if the issuers’ reported total annual earned premiums were
$20 million or more in the small group market outside the exchange.
Employee choice may be
offered in different ways. In general, a SHOP must allow a qualified
employer to offer its employees a choice among all QHPs available within
a specific metal tier of coverage, but may allow an employer to offer
18
Small employers and employees may also receive assistance from Navigators, who are
individuals and entities, such as community and consumer-focused nonprofit groups,
which receive grants from exchanges and provide information and services in a fair and
impartial manner to enrollees or potential enrollees. However, CMS has noted that
Navigators have focused largely on the individual exchanges, and that brokers have
played a much more central role in the SHOPs—as they have traditionally done in the
small-group health coverage market—providing service at the time of plan selection and
enrollment and customer service throughout the plan year.
19
In general, when offering coverage though a SHOP, employers select a plan, which
becomes the employer's reference plan. Employers also decide the percentage they will
contribute to the premiums for employees who select that plan, referred to as a defined
contribution. Employees who have been offered a choice of plans are typically able to use
the amount of the defined contribution for the reference plan when paying their premiums
for a different SHOP plan.
Page 7 GAO-15-58 Small Business Health Insurance Exchanges
broader employee choices among multiple plans across different tiers.
20
According to CMS, employee choice is intended to be a fundamental new
benefit of SHOPs, in that small employers would be able to offer multiple
plans from more than one issuer of health coverage, whereas traditionally
most small employers have offered only one or a few plans from a single
issuer. SHOPs were initially required to have the capacity to allow
employers to provide employee choice beginning in 2014. However,
under a final rule issued in June 2013, the requirement that SHOPs offer
employee choice was first postponed to 2015, although SB-SHOPs
retained the option of providing employee choice in 2014. The
requirement was further postponed under a May 2014 final rule to 2016 in
states that could demonstrate that postponing employee choice would be
in the best interest of small employers and their employees and
dependents, given the likelihood that implementing employee choice
could cause issuers to price their products and plans higher than they
would otherwise due to issuers’ beliefs about adverse selection.
21
To provide an incentive for small employers to provide health insurance,
and to make insurance more affordable, PPACA established a small
business tax credit for certain eligible small employers offering coverage
to their employees.
22
20
To make it more administratively efficient for employers to provide their employees a
choice of QHP, CMS also required SHOPs to perform premium aggregation—that is, to
aggregate the QHP premiums for multiple employees enrolling in SHOP coverage,
provide the relevant employer with a single bill identifying the total amount that is due to
the one or more QHPs in which the employer’s employees are enrolled, collect the
appropriate amount from each employer, and pay the issuers of the QHPs directly.
The tax credit was available beginning in 2010, prior
to the establishment of SHOPs. However, beginning in 2014, employers
must offer coverage to their employees through the SHOP to be eligible
21
See 79 Fed. Reg. 30240, 30349-50 (May 27, 2014) (to be codified at 45 C.F.R.
§ 155.705(b)(2)-(3)). Adverse selection refers to the potential for consumers with fewer
health concerns to select certain plans—particularly those with lower premiums—and for
consumers with greater health concerns to select other, more comprehensive plans.
Applications for consideration of delaying employee choice until 2016 were due to CMS by
June 2, 2014 for FF-SHOPs. According to CMS, the agency remains committed to
implementing employee choice in all SHOPs by 2016.
22
PPACA, §§ 1421, 10105(e), 124 Stat. at 237, 906 (codified at 26 U.S.C. § 45R).
To be eligible, an employer must: (1) have fewer than the equivalent of 25 full-time
employees, (2) have an average annual employee wage below $50,000, and (3) cover at
least 50 percent of the cost of health insurance coverage for employees.
Page 8 GAO-15-58 Small Business Health Insurance Exchanges
for the credit.
23
Beginning in 2014, employers are eligible for the credit for
a maximum of 2 years.
24
PPACA directed states to establish SHOPs by January 1, 2014.
25
In
states electing not to establish and operate an SB-SHOP, PPACA
required the federal government to establish and operate an FF-SHOP in
the state.
26
For 2014, 18 states chose to operate SB-SHOPs while 33
states opted for an FF-SHOP.
27
23
The Internal Revenue Service has stated that in 2014, small employers in certain
counties in Wisconsin and Washington where SHOP plans are not offered may be eligible
for the tax credit if they offer coverage that would have qualified for the credit prior to
January 1, 2014. See Internal Revenue Service, Section 45R – Transition Relief with
Respect to the Tax Credit for Employee Health Insurance Expenses of Certain Small
Employers, Internal Revenue Bulletin: 2014-2 (Washington, D.C.: January 6, 2014).
CMS’s and states’ roles in operating
24
The tax credit offered to eligible small employers from 2010 through 2013 was smaller
than the credit offered beginning in 2014, but had no restrictions on the number of years
employers could receive the credit. From 2010 through 2013, for-profit employers were
eligible for a credit of up to 35 percent of the employers’ share of the employees’
premiums, and nonprofit employers were eligible for a credit of up to 25 percent.
Beginning in 2014, eligible for-profit employers may receive a credit of up to 50 percent of
the employers’ share of the employees’ premiums, and nonprofit employers meeting the
eligibility criteria may receive a credit of up to 35 percent. The maximum credit is available
to employers with 10 or fewer employees and with an average annual employee wage of
$25,000 or less, and the size of the credit employers are eligible for decreases as
employer size and average employee wage increase.
25
PPACA, § 1311(b)(1), 124 Stat. at 173 (codified at 42 U.S.C. § 18031(b)(1)).
26
PPACA, § 1321(c), 124 Stat. at 186 (codified at 42 U.S.C. § 18041(c)).
27
The 18 states that had SB-SHOPs in 2014 were California, Colorado, Connecticut,
Hawaii, Kentucky, Maryland, Massachusetts, Minnesota, Mississippi, Nevada, New
Mexico, New York, Oregon, Rhode Island, Utah, Vermont, Washington, and the District of
Columbia.
CMS officials noted that Idaho, although initially approved as an SB-SHOP state, used the
FF-SHOP platform in 2014. We therefore refer to Idaho as having an FF-SHOP in 2014
for the purposes of our report. Including Idaho, the 33 states that had FF-SHOPs in 2014
were Alabama, Alaska, Arizona, Arkansas, Delaware, Florida, Georgia, Idaho, Illinois,
Indiana, Iowa, Kansas, Louisiana, Maine, Michigan, Missouri, Montana, Nebraska, New
Hampshire, New Jersey, North Carolina, North Dakota, Ohio, Oklahoma, Pennsylvania,
South Carolina, South Dakota, Tennessee, Texas, Virginia, West Virginia, Wisconsin, and
Wyoming. Some states were approved by CMS to assist with certain FF-SHOP functions
associated with consumer assistance and plan management.
These states differ from the SB-SHOP and FF-SHOP states presented in our June 2013
report (GAO-13-614) because Idaho had an FF-SHOP according to our definition, while
Mississippi operated an SB-SHOP, in 2014.
Page 9 GAO-15-58 Small Business Health Insurance Exchanges
SHOPs and individual exchanges may change in future years. CMS
officials stated that as of September 2014, Nevada was planning to begin
using the FF-SHOP platform, while Idaho was planning to begin using its
own state-based platform, in 2015.
Though SHOPs were operational in all states as of June 1, 2014, many
expected features were not yet available for a number of SHOPs.
Enrollment for the SB-SHOPs, as of June 1, 2014 for most states, has
been lower than expected, and CMS officials said they do not expect the
enrollment trends for the FF-SHOPs to be significantly different, although
they are still in the process of collecting enrollment data. Most SHOPs
had multiple plans available in each county, though in some states there
were a few counties with no plans available. Premiums varied across
states, though were generally comparable to premiums for small group
plans within the same state offered outside of the SHOPs.
All of the FF-SHOPs and most of the SB-SHOPs were operational as
required—that is, accepting enrollment applications—as of October 1,
2013. According to CMS, four of the SB-SHOPs—Hawaii, Maryland,
Mississippi, and Oregon—were not operational as of the October 1, 2013,
deadline, although all have since become operational. Hawaii became
operational on October 15, 2013, Maryland became operational on
April 1, 2014, and Oregon and Mississippi became operational on
May 1, 2014.
Websites where employers could review plan information, including
premiums and benefits, were available on October 1, 2013, for all FF-
SHOPs and most SB-SHOPs. This information allows employers and
employees to make meaningful comparisons about available SHOP plans
in their state. Plan information for the FF-SHOPs was provided by CMS
through its website. According to CMS, on October 1, 2013, the SB-
SHOPs in Maryland, Oregon, and Mississippi lacked websites where
employers could review plan and premium information. Mississippi has
since added plan and premium information to its websites. Oregon and
Maryland have directed employers to contact agents and brokers or
issuers to review plan options.
SHOPs Were
Operational in All
States, Although
Many Expected
Features Were Not
Yet Available and
Enrollment Was Low
as of June 2014
SHOPs Were Operational
in All States, Although
Many Expected Features
Were Not Yet Available,
Particularly for the
Federally Facilitated
SHOPs
Page 10 GAO-15-58 Small Business Health Insurance Exchanges
According to CMS, most SB-SHOPs created online enrollment portals by
October 1, 2013, though a handful of states—Maryland, Oregon,
California, and Mississippi—did not have online enrollment portals
available or had to take them offline, requiring employers to enroll directly
through issuers. For example, the California SHOP initially offered online
enrollment but took its enrollment portal down in February 2014 due to
technical challenges, leaving small businesses in California able to enroll
in SHOP plans only through direct enrollment. Online enrollment for the
Mississippi SHOP began when it became operational in May 2014, while
Maryland and Oregon have yet to implement online enrollment for their
SHOPs.
CMS did not implement online enrollment in the FF-SHOPs in 2014. As a
result, employers enrolling in any of the FF-SHOPs, starting in October
2013, had to enroll in SHOP coverage either through agents and brokers
or directly through issuers.
28
CMS is currently preparing to implement
online enrollment for the FF-SHOPs for 2015, and expects to launch
online enrollment fully in all FF-SHOPs by November 15, 2014, when
SHOP enrollment begins for 2015.
29
The online enrollment system will
allow, among other functions, enhanced features for agents and brokers,
notification to employees of their employers’ annual open enrollment
period, online employer payments, transmitting of enrollment and
payment transactions to issuers, and the processing of coverage
changes.
30
According to CMS, fifteen SB-SHOPs offered employee choice in 2014
through a variety of approaches, though employee choice was delayed
for the FF-SHOPs until 2015. These approaches included enabling
28
CMS and other stakeholders we interviewed noted that small employers have
traditionally used direct enrollment methods, such as working with agents and brokers, to
apply for small group coverage.
29
In preparation for launching online enrollment, CMS planned to partially launch online
enrollment early in five FF-SHOP states (Delaware, Illinois, Missouri, New Jersey, and
Ohio) in October 2014. Employers were to be able to log in, create an account, and
complete the eligibility application, or authorize an agent or broker to assist with signing up
for SHOP coverage.
30
CMS plans to add functionality to support its online system in early 2015, including
enhanced call center access to assist employers, employees, and agent and brokers;
integration with the other exchange systems to facilitate IRS reporting and data analytics;
and the handling of coverage terminations and delinquent payments.
Page 11 GAO-15-58 Small Business Health Insurance Exchanges
employers to offer a choice of plans across all metal tiers and all issuers;
a choice of plans across one metal tier but for multiple issuers; or a
choice of plans from one issuer but across multiple metal tiers. Some
states allowed the employer to choose which employee choice model to
use, while other states only offered one approach. Four states, including
California, required that employers offer their employees a choice of
plans, while others, including Rhode Island and Kentucky, gave
employers the option of choosing one plan or offering wider plan choice to
their employees.
The majority of enrolled employers in SB-SHOP states where data was
available took advantage of the employee choice feature. For example,
exchange officials in Kentucky and Rhode Island said that approximately
65 and 61 percent of enrolled employers, respectively, decided to offer
their employees a choice of plans.
31
CMS did not offer employee choice in the FF-SHOPs in 2014 but plans to
do so for many FF-SHOPs for 2015. However, CMS offered state
insurance commissioners the chance to recommend whether or not
employee choice should be implemented in their state for 2015 or
delayed until 2016, if the commissioners could adequately explain that
this would be in the best interest of small employers and their employees
In Rhode Island, in cases where
employers offered the choice of any plans through the SHOP, just over
50 percent of their employees chose the reference plan the employer had
selected, 14 percent selected a different plan within the same tier,
13 percent purchased a lower metal tier—or less expensive—plan than
the reference plan, and 21 percent purchased a higher metal tier—or
more expensive—plan than the reference plan. CMS officials said that
two additional SB-SHOPs, Colorado and New York, reported that a
majority of employers decided to offer their employees a choice of plans.
However, three SB-SHOPs did not offer employee choice in 2014:
Maryland, Massachusetts, and Oregon. Massachusetts was unable to
offer employee choice because its online system for employee choice is
still in development, according to CMS officials. Maryland and Oregon
were unable to offer employee choice because SHOP enrollment was
only available through direct enrollment, according to CMS and state
officials, respectively.
31
The remaining employers offered their employees one SHOP plan. All employers
offering coverage through California’s SHOP offered employee choice, as this was a
requirement for participating in the state’s SHOP.
Page 12 GAO-15-58 Small Business Health Insurance Exchanges
and dependents.
32
Fourteen FF-SHOP states chose to allow CMS to
implement employee choice for 2015 while 18 FF-SHOP states chose to
delay employee choice until 2016.
33
(See app. I for additional details on
SHOP functionality as of June 1, 2014.)
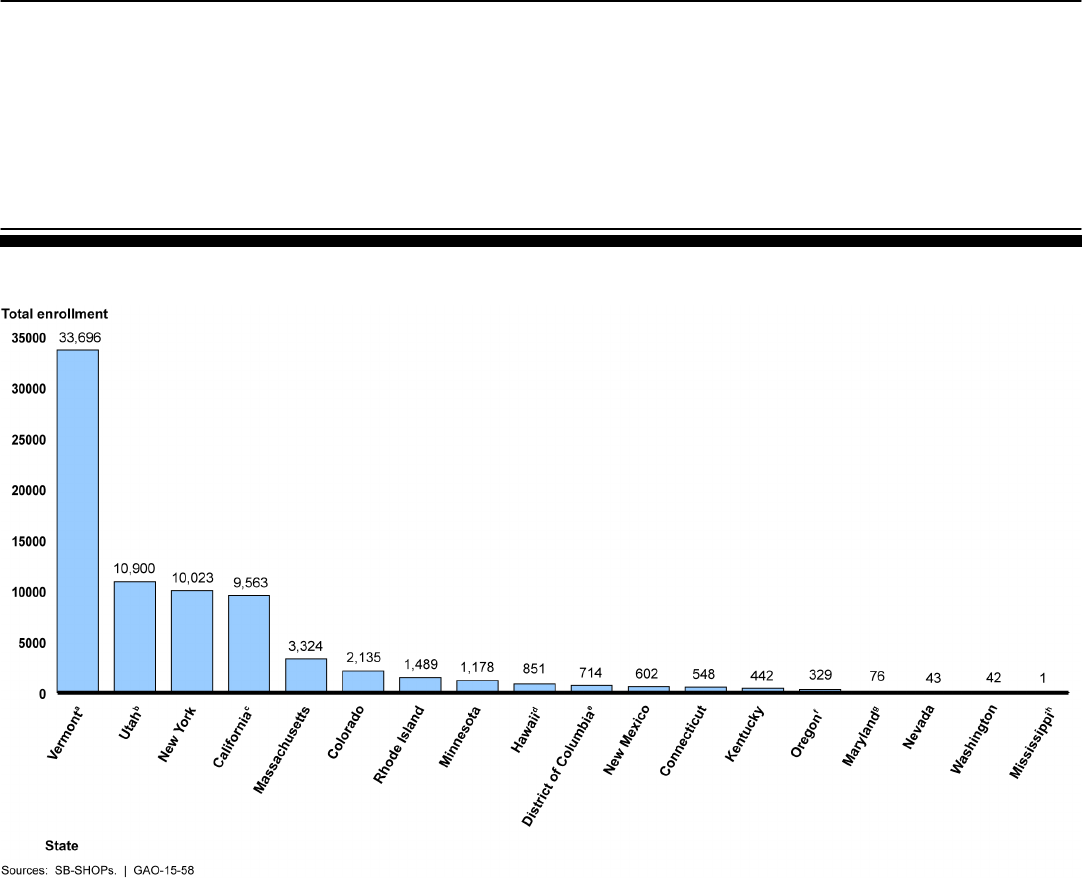
SB-SHOP plans had enrolled approximately 76,000 individuals—including
employees, spouses, and dependent children—into plans purchased
through 11,742 small employers, as of June 1, 2014 for most states, with
end dates ranging from May to September 2014. Enrollment varied widely
among the 18 states with SB-SHOPS, from 33,696 individuals (purchased
through 3,580 small employers) in Vermont,
34
to 1 individual (purchased
through 1 small employer) in Mississippi.
35
(See fig. 1.)
32
79 Fed. Reg. 30240, 30349-50 (May 27, 2014) (to be codified at 45 C.F.R.
§ 155.705(b)(2)-(3)).
33
CMS required that FF-SHOP states notify the agency of their preference and justification
for delaying employee choice until 2016. CMS approved the delay of employee choice
until 2016 for 18 FF-SHOPs: Alabama, Alaska, Arizona, Delaware, Illinois, Kansas,
Louisiana, Maine, Michigan, Montana, New Hampshire, New Jersey, North Carolina,
Oklahoma, Pennsylvania, South Carolina, South Dakota, and West Virginia. In addition,
Nevada, an SB-SHOP in 2014, will use the FF-SHOP platform in 2015 and will not offer
employee choice. The 14 FF-SHOP states that chose to allow CMS to implement
employee choice for 2015 were Arkansas, Florida, Georgia, Indiana, Iowa, Missouri,
Nebraska, North Dakota, Ohio, Tennessee, Texas, Virginia, Wisconsin, and Wyoming.
34
Vermont required that all small group plans in the state be offered only through the
SHOP.
35
Mississippi provided enrollment information as of July 1, 2014. Mississippi’s SHOP did
not come online until May, which limited the time that small employers have had to enroll.
State-Based SHOP
Enrollment Was
Significantly Lower than
Anticipated, While
Enrollment Data for
Federally Facilitated
SHOPs Were Not Yet
Available
Page 13 GAO-15-58 Small Business Health Insurance Exchanges
Figure 1: Total Enrollment in the State-Based Small Business Health Options Programs (SB-SHOPs) Generally As of June 1,
2014
Notes: Figure indicates the total number of individuals (including the employees, spouses, and any
dependent children) covered by SB-SHOP plans.
a
Vermont required that all small group plans in the state be offered only through the SHOP. Vermont
provided data as of June 13, 2014.
b
Utah had an operational exchange for small employers prior to the enactment of the Patient
Protection and Affordable Care Act.
c
California provided data as of May 22, 2014.
d
The number for Hawaii only reflects the number of employees covered, as total enrollment was not
available.
e
The number for the District of Columbia does not include Congressional employees who are required
to obtain coverage through the District of Columbia’s SB-SHOP in order to receive a government
contribution toward their health insurance premiums under the Federal Employees Health Benefits
Program.
f
The number for Oregon only reflects the number of employees covered, as total enrollment was not
available.
g
Maryland provided data as of September 15, 2014.
h
Mississippi provided data as of July 1, 2014.
Page 14 GAO-15-58 Small Business Health Insurance Exchanges
Based on the average number of employees who enrolled in each state
per small employer, it appears that the employer groups that enrolled in
the SHOPs generally had few employees, particularly given that states
allowed employers with as many as 50 employees to enroll in the SHOPs
in 2014. Overall, the average number of employees per employer was
3.7, although the average number of employees enrolled per employer in
each state varied. Employers that enrolled in Utah had the largest
average number of employees enrolled per employer, 8.3, while New
York had the smallest average number of employees enrolled per
employer, 1.6.
36
Based on official estimates and stakeholders’ expectations, SB-SHOP
enrollment—as of June 1, 2014 for most states, with end dates ranging
from May to September 2014—was significantly lower than anticipated
and, at its current pace, is unlikely to reach expectations by the end of
2014.
(See app. II for additional details on SB-SHOP
enrollment.)
37
In April 2014, the Congressional Budget Office (CBO) estimated
that 2 million employees would enroll in coverage through the SB-SHOPs
and FF-SHOPs in 2014, with the number of enrollees rising to 3 million in
2015 and leveling off at 4 million enrollees by 2017.
38
36
Mississippi is a unique situation in that only one employer enrolled and so was not
included in this calculation.
In general,
stakeholders we spoke with said that SHOP enrollment has been low,
often lower than anticipated. For example, officials from the three SB-
SHOPs we spoke to all said that enrollment has been low, with officials
from two of the states indicating enrollment was lower than expected.
Officials from the third state said challenges related to implementation
and the lack of resources for marketing the SHOP had already lowered
their expectations for enrollment, though they acknowledged that
enrollment was generally low. Further, other stakeholders, including
issuer, employer, and agent and broker representatives, also said that
enrollment to date has been lower than anticipated.
37
CMS officials cautioned against inferring future enrollment trends from the partial-year
enrollment data for 2014. Officials said that employers may enroll in the SHOPs at any
point in the year, unlike individuals pursuing coverage in the individual exchanges, which
have limited open enrollment periods. According to the officials, more employers will likely
become eligible for SHOP coverage in later months, when their existing non-SHOP plans
end.
38
See Congressional Budget Office, Updated Estimates of the Effects of the Insurance
Coverage Provisions of the Affordable Care Act (Washington, D.C.: April 2014).
Page 15 GAO-15-58 Small Business Health Insurance Exchanges
Enrollment data for the FF-SHOPs was not yet available, though CMS
officials reported that the agency was in the process of collecting the data
from issuers. According to officials, because CMS was not ultimately
prepared to implement online enrollment it has had to require each issuer
involved in an FF-SHOP to manually report enrollment data. This data
reporting role for issuers had not originally been anticipated, and so CMS
has had to work with issuers to develop protocols to submit the data.
CMS officials said that they are working on a system through which
issuers can report their 2014 SHOP enrollment data, and that they expect
to have initial data by fall of 2014 but will not have complete data for 2014
until early 2015.
39
However, CMS officials said they do not have reason to
expect major differences in enrollment trends for 2014 between the SB-
SHOPs and the FF-SHOPs. Beginning in 2015, CMS officials said they
plan to have online enrollment that will likely facilitate the more timely and
accurate collection of enrollment data.
40
39
CMS officials noted that some issuers have reported to CMS that they are unable to
accurately report complete enrollment data for 2014, which could underestimate actual
enrollment numbers ultimately reported to CMS later in 2014.
40
While enrollment data is not available for FF-SHOPs, employers that are interested in
applying for the small business tax credit in 2014 must submit paper applications to CMS
to obtain an official SHOP eligibility determination. CMS reported that it had received
12,376 paper applications from employers for FF-SHOPs as of September 8, 2014.
According to CMS officials, employers that are interested in the tax credit have up to one
year after enrolling in the SHOP to submit their paperwork to CMS. As a result, the
number of paper applications for the SHOP tax credit as of September 8, 2014 likely
differs from the actual number of employers that plan to apply for the tax credit in 2014. In
addition, as some enrollees in the SHOP may not be eligible for or interested in applying
for the tax credit, the number of paper applications likely differs from actual employer
enrollment in the FF-SHOPs.
Page 16 GAO-15-58 Small Business Health Insurance Exchanges
In nearly all states, multiple issuers offered multiple plans in the SHOPs in
2014. The total number of participating issuers and plans in each state
varied widely from 1 to 13 issuers and 3 to 320 plans.
41
Forty-five states
had more than one issuer participating in their SHOP and 31 states had 3
or more participating issuers and each issuer offered, on average, 12
plans in each rating area.
42
In looking at silver-tier plans specifically, we found that most states had at
least one silver-tier plan available in each county, though New York,
Washington, and Wisconsin had counties where no silver-tier plans were
available.
43
The type of plan with the highest enrollment also varied across SB-SHOP
states, as did the proportion of employees enrolling in these plans.
Further, most states had at least two silver-tier plans available
in each county. When looking at the total number of silver-tier plans,
Washington, D.C., offered the most, with 89, while Arkansas, New
Hampshire, and West Virginia each only had one silver-tier plan available.
Regarding issuer participation in the SHOPs, we found that just over half
of states offered silver-tier plans from two or more issuers in each county.
Maryland had the most issuers offering silver-tier plans in its SHOP, with
13, though six states—Arkansas, Mississippi, New Hampshire, North
Carolina, Washington, and West Virginia—had only one issuer offering
silver-tier plans.
44
41
For additional details on issuer participation in both the individual and small business
exchanges beginning in 2014, as well as how this compares with issuer participation in the
individual and small group markets prior to the exchanges, see GAO, Patient Protection
and Affordable Care Act: Largest Issuers of Health Coverage Participated in Most
Exchanges, and Number of Plans Available Varied,
The
highest enrollment plans in each state were most often gold-tier. The plan
with the highest enrollment was a gold-tier plan in seven states, a silver-
GAO-14-657 (Washington D.C.:
August 29, 2014)
42
PPACA required each state to establish geographical rating areas that all issuers in the
state must use as part of their rate setting. In some states these rating areas are based on
counties, while in others they are based on Metropolitan Statistical Areas.
43
As noted previously, PPACA requires that issuers participating in the SHOP offer, at a
minimum, plans at both the silver and gold levels of coverage.CMS officials said that they
expect SHOP plans to be offered in these counties in plan year 2015.
44
Enrollment data for the FF-SHOPs was not yet available, though CMS officials reported
that the agency was in the process of collecting the data from issuers.
Most SHOPs Have
Multiple Plans Available in
Each County, and Plan
Premiums Varied Across
States and Were
Generally Comparable to
Similar Plans Outside the
SHOPs
Page 17 GAO-15-58 Small Business Health Insurance Exchanges
tier plan in five states, and a platinum-tier plan in five states.
45
The
proportion of individuals enrolled in the highest enrollment plan ranged
from approximately one-fourth of enrollees in California, Connecticut,
Kentucky, and Vermont to less than 10 percent in Minnesota, New
Mexico, New York, and Utah.
46
Premiums for silver-tier plans varied within and across states,
(See app. II for additional details on the
highest enrollment SB-SHOP plans.)
47
though no
clear patterns emerged. Monthly silver-tier plan premiums for enrollees
aged 21 ranged widely from $138 for the least expensive Hawaii plan to
$523 for the most expensive Alaska plan, with the median plan costing
$262.
48
For enrollees aged 40, the monthly premiums varied from $176
for the least expensive Hawaii plan to $669 for the most expensive Alaska
plan, with the median plan costing $335. Finally, for enrollees aged 60,
the monthly premiums varied from $375 for the least expensive Hawaii
plan to $1421 for the most expensive Alaska plan, with the median plan
costing $711. The differences between the premiums of the most
expensive and least expensive silver-tier plans within a given state also
varied widely. Arizona had the largest difference, with the most expensive
plan costing almost three times as much as the lowest-cost plan.
49
North
Carolina had the least disparate silver-tier plan premiums, with the most
expensive plan costing only approximately five percent more than the
least expensive plan.
50
45
Mississippi was excluded from this summary because it only had one enrollee as of
July 1, 2014.
(See app. III for additional details about SHOP
premium variation across states.)
46
Mississippi was excluded from this analysis because it only had one enrollee as of
July 1, 2014. Hawaii and Oregon were excluded because they were unable to provide
total enrollment, and Washington was excluded because it was unable to provide total
enrollment for the highest enrollment plan.
47
We focused our analysis of plan premiums on silver-tier plans.
48
Vermont does not allow variation in plan premiums based on age and so was not
included in these comparisons.
49
As would be expected, this difference was consistent across Arizona plans for all three
age groups that we reviewed.
50
Similar to Arizona, this difference was consistent across North Carolina plans for all
three age groups that we reviewed.
Page 18 GAO-15-58 Small Business Health Insurance Exchanges
In the three states where we compared SHOP premiums to non-SHOP
small group market premiums in the state, we found that premiums for
silver-tier plans were generally comparable.
51
PPACA requires that prices
for identical plans within a given state be the same, regardless of whether
plans are offered on or off the SHOP.
52
Many stakeholders we spoke to
said that SHOP premiums were generally comparable to premiums for
plans outside of the SHOPs. As previously noted, PPACA requires that
small group plans meet a number of requirements. These requirements
limit the overall variability between PPACA-compliant plans offered within
or outside of the SHOPs, including variation in premiums.
Stakeholders we interviewed reported that the primary incentive for
employers to use the SHOPs has been the small business tax credit.
However, stakeholders identified several factors that may have hindered
enrollment, thus leading to current low SHOP enrollment. Stakeholders
also described factors that may help stimulate or detract from SHOP
enrollment in the future.
51
For California, the prices for non-SHOP plans were somewhat higher than the prices for
SHOP plans, with the lowest priced, the median priced, and the highest priced plan in the
non-SHOP market being somewhat higher than the lowest priced, the median priced, and
the highest priced plan in the California SHOP. For Illinois, the highest priced plan in the
non-SHOP market was somewhat more expensive than the highest priced plan in the
Illinois SHOP.
We requested data from the five states that we selected to interview state-level
stakeholders, California, Illinois, Kentucky, Rhode Island, and Texas. The necessary data
were not available within our timeframes from Kentucky and Texas.
52
PPACA, § 1301(a)(1)(C)(iii) (codified at 42 U.S.C. 18021(a)(1)(C)(iii)).
Stakeholders
Identified Several
Factors That May
Have Led to Current
Low SHOP
Enrollment and That
May Affect Future
Enrollment Growth
Page 19 GAO-15-58 Small Business Health Insurance Exchanges
Many stakeholders, including issuer, employer, and agent and broker
representatives we interviewed, reported that the primary incentive for
employers to use SHOPs has been the small business tax credit.
53
Employers must generally purchase coverage through a SHOP and meet
certain other criteria, including having fewer than 25 employees, to be
eligible for the credit, which they may receive for a maximum of two years
beginning in 2014. Most employer group representatives reported that
those small employers that were interested in and taking steps to enroll in
the SHOPs were largely doing so in order to be eligible for the tax credit.
Exchange officials in Kentucky also reported that the tax credit has likely
been an important incentive for small employers enrolling in the state’s
SHOP, and that most employers that had enrolled as of April 2014 had
less than 25 employees, indicating that they may have been pursuing the
credit.
54
Similarly, as discussed previously, we found that the average
number of enrolled employees in SB-SHOPs ranged from 1.6 to 8.3
employees,
55
However, several stakeholders noted that the tax credit is too small and
administratively complex to motivate many small employers to enroll.
CMS officials and one employer group representative noted that the
temporary nature of the tax credit—that is, the fact that employers may
receive the credit for only 2 years beginning in 2014—may deter some
employers from offering coverage for the first time through the SHOP to
obtain the credit. This is consistent with our prior work, which revealed
low use of the credit even prior to the establishment of the SHOPs. In
2012, we reported that the take-up of the small business tax credit in tax
year 2010, the first year the credit was offered, was much lower than the
estimated number of eligible employers. According to tax preparers and
other stakeholders we interviewed for that work, small employers likely
did not view the credit as a sufficient incentive to begin offering health
suggesting that many enrolled employers may have been
eligible for the credit.
53
The Internal Revenue Service has stated that in 2014, small employers in certain
counties in Wisconsin and Washington where SHOP plans are not offered may be eligible
for the tax credit if they offer coverage that would have qualified for the credit prior to
January 1, 2014.
54
Kentucky exchange officials noted that they cannot determine how many employers
have applied for or received the tax credit because the federal government, rather than
the state, handles tax credit applications.
55
Mississippi is a unique situation in that only one employer enrolled and so was not
included in this calculation.
Stakeholders Reported
that the Small Business
Tax Credit Has Been the
Primary Motivator for
Employers to Enroll in
SHOPs
Page 20 GAO-15-58 Small Business Health Insurance Exchanges
insurance, particularly given the complexity of, and time required to claim,
the credit.
56
Although the small business tax credit may have led some employers to
enroll in the SHOPs, stakeholders identified several other factors that
may have hindered enrollment, thus leading to current low SHOP
enrollment.
• Delays in key SHOP features. Stakeholders, including
representatives of national employer, agent and broker, and insurance
commissioner groups, said that the delays in implementation of online
enrollment and employee choice in the FF-SHOPs may have hindered
SHOP enrollment. These key features, which have also been delayed
in certain SB-SHOPs, are not typically available to small employers
purchasing coverage through other means. According to
stakeholders, until these key features are implemented, employers
may not have as much incentive to enroll in coverage through the
SHOP.
• Limited awareness of and misconceptions about SHOP
availability. Many stakeholders, including state exchange officials
and national- and state-level agent, broker, and employer
representatives, reported a lack of employer awareness of the ability
to enroll in SHOP plans beginning October 1, 2013, largely due to
misconceptions about whether the SHOPs were open for enrollment
and a lack of outreach by states and CMS. Stakeholders said that
media reports announcing delays in certain SHOP features—in
particular, the delays in FF-SHOP online enrollment and employee
choice—led many employers to assume that the overall
implementation of SHOPs was delayed and that enrolling in plans was
not yet possible. In addition, stakeholders said that low awareness
stemmed from a federal and state emphasis on highlighting the
availability of the individual exchanges. For example, exchange
officials from one SB-SHOP state noted that employer awareness of
56
See GAO, Small Employer Health Tax Credit: Factors Contributing to Low Use and
Complexity, GAO-12-549 (Washington, D.C.: May 14, 2012). CMS officials noted that the
agency launched a SHOP Small Business Health Care Tax Credit Estimator, available at
the federal exchange website, in early 2014 to ease administrative burden and help
employers better understand the tax credit. According to the officials, this tool is intended
to make it easier for employers to determine if they qualify for the tax credit as well as the
size of the credit they might receive.
Stakeholders Identified
Several Factors That May
Have Hindered Current
SHOP Enrollment
Page 21 GAO-15-58 Small Business Health Insurance Exchanges
the SHOP remained low in part because the state initially focused
outreach and marketing efforts on the individual exchange. However,
exchange officials from this and another SB-SHOP state reported that
with the end of their individual exchanges’ open enrollment periods,
the states are now focusing outreach and marketing efforts on their
SHOPs, which must provide for rolling enrollment.
57
• Renewal of existing, noncompliant plans. The majority of
stakeholders—including national-level groups as well as stakeholders
representing four of the five states included in our study—said that the
ability for employers to renew their existing, non-PPACA compliant
plans may have limited SHOP enrollment.
58
National-level employer
and agent and broker groups we interviewed said that most small
employers chose to renew their existing plans in states where this
was permitted, in part due to a general preference for the status quo,
as well as other factors, such as concerns about potential premium
increases associated with new plans.
59
• Technical challenges and administrative burden. Some
stakeholders said that the ongoing technical challenges and
administrative burden associated with many of the SHOPs have
served as a barrier to entry for employers, in part by discouraging
some agents and brokers from recommending the SHOP to
employers. National- and state-level employer group representatives
reported hearing from small employers that they have avoided SHOPs
due to technical challenges with SHOP websites, as well as
administrative burdens, such as difficulty reaching customer service
and, in some cases, the need to send application paperwork by mail.
State exchange officials reported that they worked closely with agents
Kentucky, California, and
Illinois exchange officials, as well as CMS officials who participated in
the implementation of the SHOP in Illinois and Texas, said that the
renewal of these plans may have limited SHOP enrollment in these
states.
57
The open enrollment period refers to the limited time frame when individuals are eligible
to enroll in QHPs through an individual exchange. Individuals may be eligible to enroll in
QHPs outside of the open enrollment period if they experience certain qualifying life
events.
58
Rhode Island exchange officials indicated that this factor was not applicable in Rhode
Island as it did not permit the renewal of non-PPACA-compliant plans in 2014.
59
In addition, press reports have suggested that some issuers may have encouraged their
customers to renew their noncompliant plans early, before SHOP enrollment and pricing
became available.
Page 22 GAO-15-58 Small Business Health Insurance Exchanges
and brokers to establish their SB-SHOPs, particularly given that most
small employers have traditionally relied on agents and brokers when
purchasing coverage for their employees. However, state exchange
officials and other stakeholders, including CMS officials, noted that
agents and brokers still faced challenges associated with using
SHOPs. These challenges included, in some cases, poor or
inaccessible customer service for brokers; poor training for brokers on
SHOP requirements; the extra time required to explain SHOP
requirements to clients; challenges receiving compensation; and the
lack of a dedicated broker “portal” on some SHOP websites that
would allow brokers to set up and help manage accounts for their
clients.
60
Agent and broker representatives from one state noted that
challenges such as these have led some agents and brokers to avoid
recommending that their small employer clients use the SHOP.
Despite the various factors that may have restrained SHOP enrollment to
date, many stakeholders noted that certain other factors suggest that the
SHOPs have the potential to experience future enrollment growth.
According to some stakeholders, central to enrollment growth will be the
phasing out of noncompliant plans, the resolution of the technical
challenges and reduction of the administrative burden cited as hampering
current enrollment, and the demonstration of a “value proposition” that
gives employers a reason for preferring SHOP-based coverage to
coverage available outside the SHOP. Stakeholders suggested several
additional factors that could help stimulate future SHOP enrollment
growth.
• Improved coordination with agents and brokers. Stakeholders,
including CMS officials, state exchange officials, and issuer,
employer, and agent and broker representatives, emphasized the
importance of coordinating with and providing improved web- or
phone-based tools to agents and brokers in order to facilitate SHOP
enrollment. States and CMS reported taking steps to resolve certain
challenges faced by agents and brokers when using the SHOP. For
example, Kentucky exchange officials said that they are working to
develop a tool that will allow agents and brokers to easily provide
60
The FF-SHOPs offered customer service phone lines, but not broker portals; however,
CMS officials indicated that FF-SHOPs will offer broker portals when online enrollment
begins in November 2014.
Stakeholders Identified
Various Factors That Have
the Potential to Contribute
to or Detract from Future
SHOP Enrollment Growth
Page 23 GAO-15-58 Small Business Health Insurance Exchanges
price quotes across multiple SHOP plans to their clients, and are
considering allowing SHOP-certified agents and brokers to initiate
applications on behalf of employers. Illinois exchange officials
reported developing a dedicated section for agents and brokers on the
state’s SHOP website through which agents and brokers can obtain
updated information on the SHOP, in response to feedback from
agent and broker community leaders. CMS officials said that
establishing a broker portal for the FF-SHOPs is a key agency priority,
and that the agency plans to have a broker portal in place when FF-
SHOP online enrollment becomes available in fall 2014. According to
CMS officials, the portal will, among other functions, allow agents and
brokers to search for and communicate with employer clients; monitor
employees’ enrollment progress; make changes to employee rosters;
and receive messages regarding employers’ monthly invoices,
including any late payment warnings.
61
• Availability of employee choice. Some stakeholders stated that the
employee choice feature, when fully implemented in all states, will be
a key value proposition for the SHOPs. For instance, CMS officials
said that employers will likely value being able to offer employees a
choice from among multiple plan and issuer options—an ability that
small employers typically have not been able to offer. Employer group
representatives reported that their members consider employee
choice to be an important benefit of the SHOPs, as employees will be
able to decide on their own the coverage that best suits their needs
and, if necessary, will have the option to spend more to purchase
more comprehensive plans. Evidence from Kentucky and Rhode
Island, whose SHOPs offer, but do not require, the use of employee
choice, further suggests that employers may value this feature. As
discussed previously, according to state exchange officials, the
majority of employers in Kentucky and Rhode Island that enrolled in
the SHOPs chose to offer their employees the choice of multiple
plans.
62
However, some issuer representatives and other stakeholders were
uncertain about the value of employee choice, noting that it is
61
Employee rosters contain information, such as names and dates of birth, for each
employee to whom SHOP coverage is offered.
62
According to CMS officials, data reported to CMS by two additional SB-SHOP states—
Colorado and New York—indicate that the majority of employers using the SHOP in those
states have chosen to offer employee choice.
Page 24 GAO-15-58 Small Business Health Insurance Exchanges
challenging for issuers to implement and that too many choices may
be overwhelming for employers and employees. Representatives from
national issuer and insurance commissioner groups reported that it is
time consuming and expensive for issuers to build the information
technology systems required for premium aggregation and other
issuer-specific functions necessary for employee choice. In addition,
issuers and other stakeholders have reported concerns regarding
whether employee choice would lead to adverse selection among
plans in the SHOP—a concern that has, in part, led some states to
delay their implementation of employee choice until 2016.
• Increased marketing to employers. Some stakeholders said that
states need to better market the SHOP to small employers to increase
SHOP awareness. Some employer group representatives said states
need to improve outreach by more aggressively targeting small
employers and highlighting the value of the SHOPs in their marketing.
Exchange officials in one state emphasized the importance of
marketing the SHOPs to small employers as a product that offers
value, rather than performing traditional outreach, which is more
characteristic of public programs. The officials also noted that
marketing must be conducted continuously throughout the year, given
that employers renew their coverage at different points in the year.
• Robust issuer participation. Although stakeholders representing
four of the five states included in our study reported that issuer
participation has not been a challenge, CMS officials said that robust
issuer participation will be important in ensuring the SHOPs’ long-term
viability. Issuer representatives noted that, due to the requirement that
certain issuers must participate in a state’s FF-SHOP if they wish to
participate in its federally facilitated individual exchange, some issuers
will be required to participate in the SHOPs.
63
63
78 Fed. Reg. 15410, 15535 (Mar. 11, 2013) (to be codified at 45 C.F.R. § 156.200(g)).
In addition, some SB-SHOPs require that issuers meeting certain requirements participate
in the state’s SHOP.
However, according to
the representatives, other issuers may be hesitant to participate given
factors such as uncertainties regarding delays in SHOP functionality
and technical readiness; potential new requirements, such as those
related to the adequacy of provider networks; the expense and
complexity of implementing employee choice and other SHOP
features; and the ability for employers to renew noncompliant plans.
CMS officials said that although some issuers may be reluctant to
Page 25 GAO-15-58 Small Business Health Insurance Exchanges
participate in the FF-SHOPs in the early years of implementation,
once information technology systems have been fully developed and
refined, issuers may be more eager to participate.
• Expansion of the SHOPs to larger employers. Exchange officials in
one state noted that as eligibility for SHOP enrollment expands to
employers with up to 100 employees—which must occur no later than
January 1, 2016—and, eventually, to larger employers in some states,
additional employers may consider the SHOP as an option for
purchasing coverage.
64
• Financial sustainability of the SHOPs. Exchange officials in one
state noted that an essential element of SHOP viability will be
ensuring the SHOPs are financially sustainable.
However, based on the small average number
of employees per employer enrolled in SB-SHOPs, it remains to be
seen whether larger employers will enroll when given the opportunity.
65
64
CMS officials said that as of September 2014 they were not aware of any states that
were planning to expand the SHOP to employers with 51 to100 employees in 2015.
They and other SB-
SHOP exchange officials we interviewed said that their states have
proposed or finalized funding mechanisms in place. In two of the
states, these funding mechanisms will draw from either all exchange
plans—both individual and SHOP—or all health plans in the state;
therefore, low initial SHOP enrollment is not likely to significantly
Beginning in 2015, employers with 100 or more employees that do not offer affordable
health coverage to 70 percent or more of their employees may be subject to a penalty if at
least one employee receives subsidized coverage through an exchange. Beginning in
2016, employers with 50 or more employees that do not offer affordable health coverage
to their full-time employees may be subject to this penalty if at least one employee
receives subsidized coverage through an exchange. PPACA, § 1513(a). 124 Stat. at 253
(codified at 26 U.S.C. § 4980H); 79 Fed. Reg. 8544, 8575, 8597-8601 (Feb. 12, 2014) (to
be codified at 26 C.F.R. §§ 54.4980H-4, 54.4980H-5). Therefore, as SHOP eligibility
expands to larger employers and these penalties take effect, more employers may be
likely to participate in the SHOP.
65
States operating SB-SHOPs are required to ensure that the SHOPs are self-sustaining
by January 1, 2015, meaning that states must ensure their SHOPs have sufficient funding
to support ongoing operations, as federal grants awarded to establish exchanges will no
longer be available. SHOPs may generate funding for SHOP operations in certain ways,
including requiring issuers to pay user fees, or a percentage of premiums charged by the
issuer. HHS requires that issuers participating in the FF-SHOPs pay a monthly user fee to
fund FF-SHOP operations; in 2014, this fee is equal to 3.5 percent of the monthly
premium charged by the issuer. HHS requires that this user fee be spread across all of an
issuer’s small group plans, regardless of whether the plans are offered in a SHOP.
Page 26 GAO-15-58 Small Business Health Insurance Exchanges
affect SHOP operating revenues in those states.
66
Stakeholders also described factors whose future effects on SHOP
enrollment are more uncertain or have the potential to detract from SHOP
enrollment growth in the long term.
However, one
stakeholder expressed concern regarding whether SHOPs will be
sustainable in the long run if enrollment remains low, particularly given
the expense required to maintain the SHOPs’ information technology
systems.
• Loss of the tax credit. As noted previously, stakeholders and our
analysis of SB-SHOP enrollment data suggested that many
employers currently enrolling in the SHOP may be eligible for the tax
credit. However, employers may only receive the tax credit for a
maximum of 2 years. It therefore remains to be seen whether
employers will continue to purchase coverage through the SHOP
once they have exhausted their ability to receive the tax credit, and
how this will affect overall SHOP enrollment. One employer
representative suggested that an extension of the credit, or a re-
design of the credit such that larger businesses are eligible, will help
ensure SHOP enrollment growth moving forward.
• Comparability of prices on and off the SHOP. Issuer
representatives and other stakeholders noted that prices for SHOP
plans are likely to remain similar to prices for non-SHOP small group
plans, which may limit the incentive for small employers to enroll in
coverage through the SHOP. According to stakeholders, small
employers’ coverage decisions are largely driven by price. However,
as we noted previously, premiums are currently similar for plans
offered on and off the SHOP in part due to the requirement that prices
for identical plans in a given state be the same, regardless of whether
they are offered on or off the SHOP. In order for issuers to offer more
competitive prices through the SHOPs, they must offer unique,
SHOP-only plans that are lower in price when compared to non-
SHOP options. However, according to issuer representatives, there
are limited mechanisms by which issuers could do so. As PPACA
requires that all plans offer a set of minimum essential health benefits,
issuers are limited in the extent to which they can lower prices by
66
Exchange officials in the remaining SB-SHOP state noted that they have proposed
various options for SHOP funding, but that they expect that operating revenues and
expenditures for the state’s individual exchange and SHOP will be combined.
Page 27 GAO-15-58 Small Business Health Insurance Exchanges
restricting the benefits they offer in SHOP plans. In addition, though
issuers could lower prices for SHOP plans by offering narrower
provider networks, issuer representatives cite the high administrative
costs of creating and maintaining new networks as a deterrent.
• Competition with private exchanges. Some stakeholders, including
issuer, agent, and broker representatives, as well as exchange
officials from one state, reported that private exchanges for small
group coverage—or online health coverage marketplaces managed
by private companies, such as issuers or benefits consulting firms—
are becoming more prevalent and may compete with SHOPs for
employer enrollment. According to some agent and broker
representatives, private exchanges may appeal to employers
because, in some cases, they offer employee choice—a key value
proposition of the SHOP that has not yet been implemented in all
states—without many of the requirements associated with the SHOP.
Exchange officials from one state said that recently created private
exchanges in that state have been able to spend more on advertising,
which has made it difficult for the SHOP to compete. However, the
officials noted that the SHOPs provide increased value in that they
offer full transparency and choice of SHOP plans—whereas some
private exchanges, despite claiming to offer full choice of plans,
simply offer plans from the carrier operating the exchange.
• Possibility of sending employees to the individual exchanges.
Exchange officials from two states and some agent and broker
representatives reported that some small employers have chosen, or
may choose in upcoming years, to drop coverage for their employees
altogether, particularly in light of the availability of premium and cost-
sharing assistance for eligible low- and moderate-income individuals
obtaining coverage through an individual exchange. CMS officials said
they have heard anecdotal information that this may be occurring, but
have no data. Several recent employer surveys have found that, while
the majority of surveyed small employers were not considering
dropping coverage for their employees, a minority were intending to or

Page 28 GAO-15-58 Small Business Health Insurance Exchanges
considering whether to drop coverage and, in some cases, direct their
employees to the individual exchanges in 2014 or 2015.
67
• Potential for adverse selection. If it were to occur, adverse selection
between SHOP and non-SHOP plans could lead to increased SHOP
premiums and thus inhibit SHOP enrollment in the long term.
However, issuer representatives said that the similarity in premiums
seen thus far has diminished concerns about such adverse selection.
The issuer representatives said a greater concern is the risk for
adverse selection between PPACA-compliant plans—that is, both the
SHOP and non-SHOP plans that comply with PPACA’s insurance
reforms—and the existing, noncompliant plans that have been
renewed. This risk may be temporary, as CMS’s current transitional
relief policy, under which noncompliant plans may continue to be
offered, permits issuers of such plans to offer renewals of these plans
only for plan years beginning on or before October 1, 2016.
68
67
For example, one survey found that 67 percent of respondents said they would continue
to offer health coverage in 2014, while 6 percent said they would definitely stop offering
coverage and 27 percent said they would consider discontinuing coverage under certain
circumstances. See eHealth ®, Small Employer Health Insurance Survey: March 2013,
accessed August 21, 2014,
In
addition, PPACA established mechanisms to mitigate adverse
selection if it does occur among PPACA-compliant plans, and
stakeholders said it will be at least 1 year, if not several years, before
http://news.ehealthinsurance.com/_gallery/get_file/?file_id=514a002dfc96aa2799001afe&f
ile_ext=.pdf. Another survey found that 23 percent of respondents were considering
dropping coverage and giving money directly to employees to purchase coverage through
the individual exchange in late 2013 or 2014. See National Small Business Association,
2014 Small Business Health Care Survey, accessed August 21, 2014,
http://www.nsba.biz/wp-content/uploads/2014/02/Health-Care-Survey-2014.pdf. An
additional survey found that the majority, or approximately 85 percent, of small employer
respondents were very or definitely likely to continue coverage for their full-time
employees in 2015, and another approximately 9 percent said that they were somewhat
likely to continue coverage. The remaining 7 percent said they were more likely to direct
employees to the individual exchanges in 2015. See International Foundation of Employee
Benefit Plans, 2014 Employer-Sponsored Health Care: ACA’s Impact (Brookfield, Wis.:
2014).
68
CMS has noted, however, that it may consider extending this transitional policy for an
additional year. See Department of Health and Human Services, Centers for Medicare &
Medicaid Services, Extension of Transitional Policy through October 1, 2016,
(Washington, D.C.: Mar. 15, 2014).
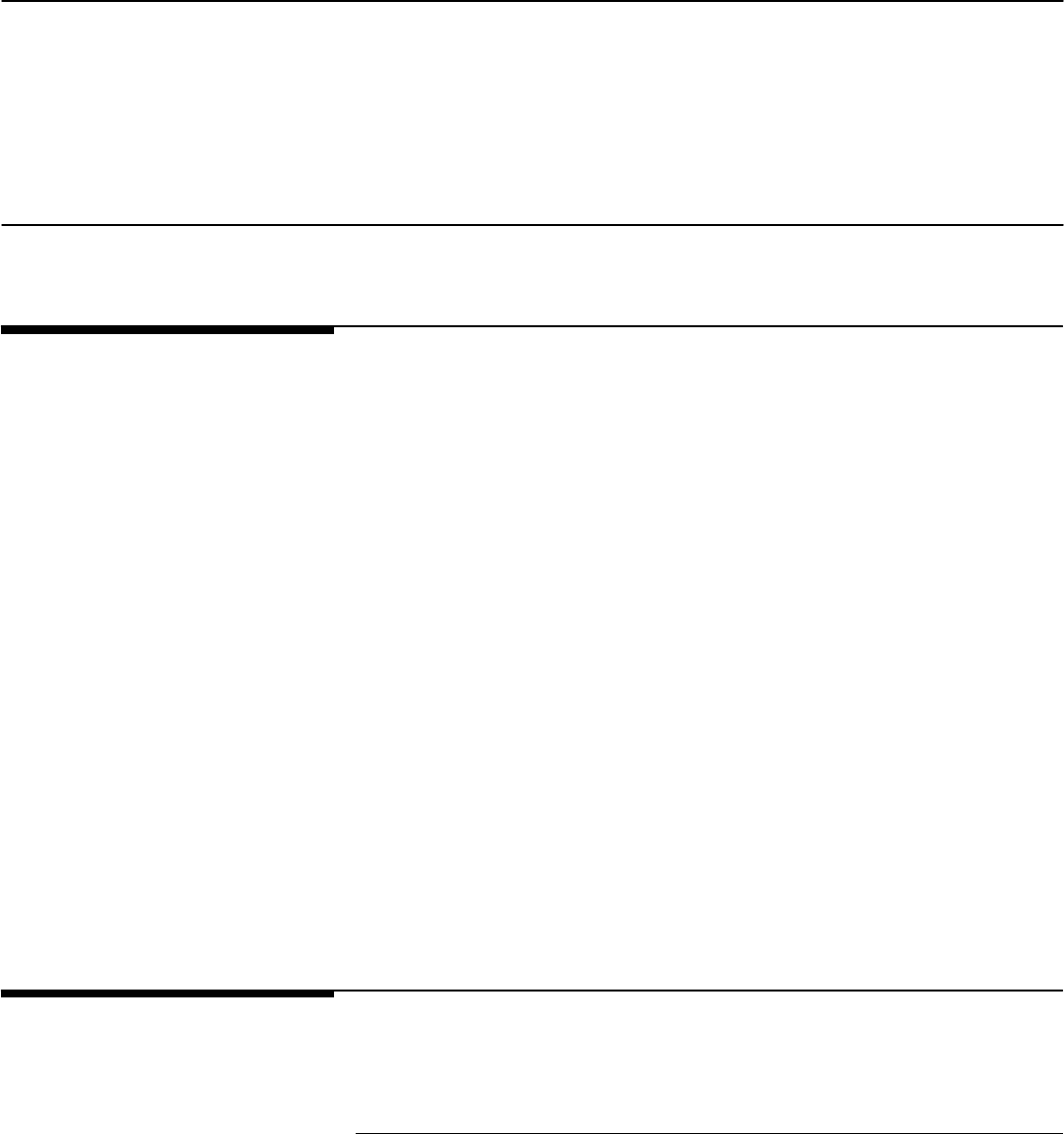
Page 29 GAO-15-58 Small Business Health Insurance Exchanges
it becomes clear if adverse selection is occurring in the SHOPs, as
well as how well these mechanisms will mitigate its effect.
69
The SHOPs are an important element of PPACA, intended to provide a
new mechanism by which small employers can shop for and purchase
health insurance coverage for their employees and to offer features not
typically available to the employees of small employers, such as the
ability to choose among multiple health plans. While much progress has
been made by CMS and states to ensure all SHOPs are now operational,
early evidence suggests enrollment is significantly lower than anticipated
amid the delayed availability of key functions among many SHOPs and
misconceptions by employers about the availability of SHOPs. CMS
officials and other stakeholders point to structural factors to help explain
the current low enrollment—such as the temporary ability for employers in
many states to renew their existing plans even if they do not comply with
PPACA insurance reforms—and suggest reasons for optimism about
future SHOP enrollment trends. They point to such factors as the phase-
out of the noncompliant plans, the expected availability of online
enrollment and employee choice functions in many more SHOPs, and
intended CMS or state efforts to improve SHOP awareness and
coordination with agents and brokers. Nevertheless, other factors may
temper such optimism, such as the loss of the small business tax credit
for some employers, the potential for adverse selection, and the
challenge SHOPs may face in competing with plans offered to small
employers outside of the SHOPs. These collective factors will vary across
states and continue to evolve, suggesting that a determination of the
long-term impact of the SHOPs remains premature at this time.
We received comments from HHS on a draft of this report (see app. V).
HHS described steps it is taking to improve the SHOP program based on
lessons learned from the first year of operation and emphasized the
69
These provisions, or risk mitigation mechanisms, are designed to mitigate the potential
effects of adverse selection and provide stability for health insurance issuers in the
individual and small group markets. All issuers in the small group market are eligible to
participate in the risk adjustment programs. Issuers of small group plans offered through a
SHOP are also eligible to participate in the temporary risk corridors program in effect in
2014, 2015, and 2016. According to issuer representatives, of these two mechanisms, risk
adjustment likely has the more significant ability to help stabilize SHOP premiums. GAO is
separately examining early experiences with these risk mitigation programs.
Concluding
Observations
Agency Comments
Page 30 GAO-15-58 Small Business Health Insurance Exchanges
future role SHOPs could play to produce more competition in the small
group health insurance markets as the SHOPs improve and mature. HHS
also provided technical comments, which we incorporated as appropriate.
We are sending copies of this report to the Secretary of Health and
Human Services and other interested parties. In addition, the report is
available at no charge on the GAO website at http://www.gao.gov.
If you or your staff have any questions about this report, please contact
John E. Dicken at (202) 512-7114 or [email protected]. Contact points for
our Offices of Congressional Relations and Public Affairs may be found
on the last page of this report. GAO staff who made key contributions to
this report are listed in appendix VI.
Sincerely yours,
John E. Dicken
Director, Health Care
Appendix I: Small Business Health Options
Program (SHOP) Features as of June 1, 2014
Page 31 GAO-15-58 Small Business Health Insurance Exchanges
SHOP
Date SHOP
enrollment
began
SHOP website
allows
browsing for
plans and
premiums
SHOP allows
employers to
enroll online
SHOP offers
employee
choice
State-based SHOPS
California 10/1/2013 ● ○
a
●
Colorado 10/1/2013 ● ● ●
Connecticut 10/1/2013 ● ● ●
District of Columbia 10/1/2013 ● ● ●
Hawaii 10/15/2013 ● ● ●
Kentucky 10/1/2013 ● ● ●
Maryland 4/1/2014 ○ ○ ○
Massachusetts 10/1/2013 ● ● ○
Minnesota 10/1/2013 ● ● ●
Mississippi 5/1/2014 ● ● ●
Nevada 10/1/2013 ● ● ●
New Mexico 10/1/2013 ● ● ●
New York 10/1/2013 ● ● ●
Oregon 5/1/2014 ○ ○ ○
Rhode Island 10/1/2013 ● ● ●
Utah 10/1/2013
b
● ● ●
Vermont 10/1/2013 ● ● ●
Washington 10/1/2013 ● ● ●
Federally facilitated SHOPs
Alabama 10/1/2013 ● ○ ○
Alaska 10/1/2013 ● ○ ○
Arizona 10/1/2013 ● ○ ○
Arkansas 10/1/2013 ● ○ ○
Delaware 10/1/2013 ● ○ ○
Florida 10/1/2013 ● ○ ○
Georgia 10/1/2013 ● ○ ○
Idaho
c
10/1/2013 ● ○ ○
Illinois 10/1/2013 ● ○ ○
Indiana 10/1/2013 ● ○ ○
Iowa 10/1/2013 ● ○ ○
Kansas 10/1/2013 ● ○ ○
Appendix I: Small Business Health Options
Program (SHOP) Features as of June 1,
2014
Appendix I: Small Business Health Options
Program (SHOP) Features as of June 1, 2014
Page 32 GAO-15-58 Small Business Health Insurance Exchanges
SHOP
Date SHOP
enrollment
began
SHOP website
allows
browsing for
plans and
premiums
SHOP allows
employers to
enroll online
SHOP offers
employee
choice
Louisiana 10/1/2013 ● ○ ○
Maine 10/1/2013 ● ○ ○
Michigan 10/1/2013 ● ○ ○
Missouri 10/1/2013 ● ○ ○
Montana 10/1/2013 ● ○ ○
Nebraska 10/1/2013 ● ○ ○
New Hampshire 10/1/2013 ● ○ ○
New Jersey 10/1/2013 ● ○ ○
North Carolina 10/1/2013 ● ○ ○
North Dakota 10/1/2013 ● ○ ○
Ohio 10/1/2013 ● ○ ○
Oklahoma 10/1/2013 ● ○ ○
Pennsylvania 10/1/2013 ● ○ ○
South Carolina 10/1/2013 ● ○ ○
South Dakota 10/1/2013 ● ○ ○
Tennessee 10/1/2013 ● ○ ○
Texas 10/1/2013 ● ○ ○
Virginia 10/1/2013 ● ○ ○
West Virginia 10/1/2013 ● ○ ○
Wisconsin 10/1/2013 ● ○ ○
Wyoming 10/1/2013 ● ○ ○
Legend: ● = Yes; ○ = No
Sources: Centers for Medicare & Medicaid Services. | GAO-15-58
a
In November 2013, California launched online enrollment for the SHOP. However, the system was
taken down in February 2014 and now California is only using direct enrollment.
b
Utah had an operational exchange for small employers prior to the enactment of the Patient
Protection and Affordable Care Act.
c
Idaho originally planned to establish an SB-SHOP, but ultimately elected to use the FF-SHOP
platform. We therefore consider Idaho as having an FF-SHOP in 2014 for the purposes of our report.
Appendix II: State-Based Small Business
Health Options Program (SB-SHOP)
Enrollment Generally as of June 1, 2014
Page 33 GAO-15-58 Small Business Health Insurance Exchanges
Highest enrollment plan
State
Employer
enrollment
Employee
enrollment
Total
enrollment
Average
employees
enrolled per
employer Metal tier
Employee
enrollment
Total
enrollment
California
a
1,360 6,667 9,563 4.9 Silver 1,749 2,499
Colorado 258 1,499 2,135 5.8 Silver 171 247
Connecticut 92 344 548 3.7 Silver 95 150
District of Columbia 211 525 714 2.5 Platinum 66 79
Hawaii
b
398 851 2.1 7a
c
228
Kentucky 58 341 442 5.9 Gold 92 124
Maryland
d
15 65 76 4.3 Gold 6 13
Massachusetts 729 1,840 3,324 2.5 Platinum 240 409
Minnesota 159 790 1,178 5.0 Gold 57 87
Mississippi
e
1 1 1 1 Gold 1 1
Nevada 16 41 43 2.6 Gold 10 10
New Mexico 129 408 602 3.2 Gold 41 57
New York
f
3,964 6,390 10,023 1.6 Platinum 637
Oregon
g
57 329 5.8 Silver 41
Rhode Island 229 884 1,489 3.9 Gold 171 286
Utah 478 3,977 10,900 8.3 Gold 303 757
Vermont
h
3,580 18,706 33,696 5.2 Platinum 4,535 8,436
Washington
i
8 25 42 3.1 Silver 9
Sources: SB-SHOPs. | GAO-15-58
Notes: Total enrollment reflects the total number of individuals (including the employees, spouses,
and any dependent children) covered by SB-SHOP plans.
a
California provided data as of May 22, 2014.
b
Hawaii was not able to provide total enrollment.
c
In Hawaii, group plans are designated as “7a” or “7b,” which are the equivalent of platinum- and
gold-tier plans, respectively.
d
Maryland provided the number of employers enrolled as of September 2, 2014, and the number of
enrollees, including the plan with the highest enrollment, as of September 15, 2014. Maryland had
two plans with 13 total enrollees; both plans were gold-tier.
e
Mississippi provided data as of July 1, 2014.
f
New York was not able to provide the number of employees enrolled for the highest enrollment plan.
g
Oregon was not able to provide total enrollment.
h
Vermont provided data as of June 13, 2014
i
Washington was unable to provide total enrollment for the highest enrollment plan.
Appendix II: State-Based Small Business
Health Options Program (SB-SHOP)
Enrollment Generally as of June 1, 2014
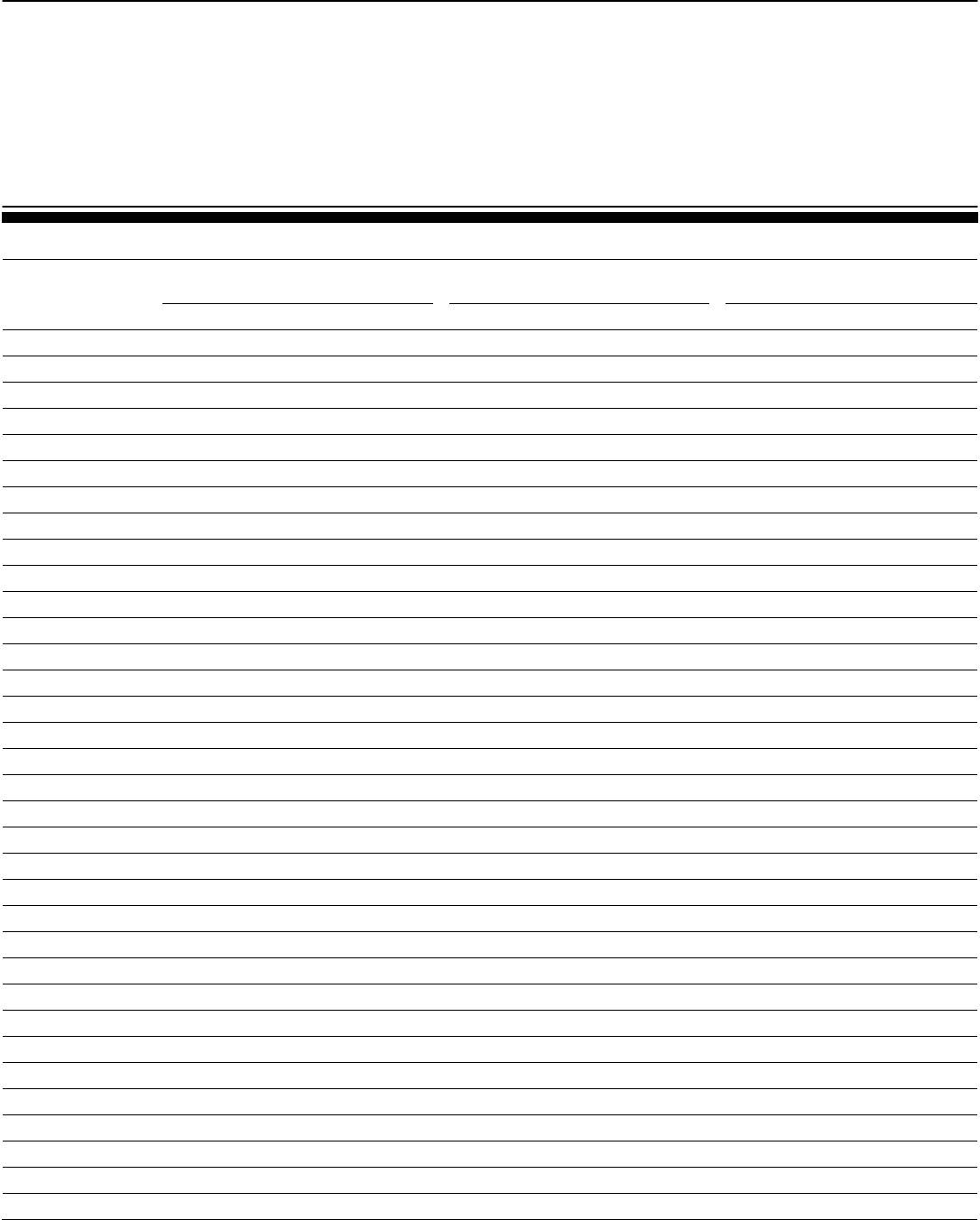
Appendix III: Small Business Health Options
Program (SHOP) 2014 Average Monthly
Premiums for Silver-Tier Plans
Page 34 GAO-15-58 Small Business Health Insurance Exchanges
Silver-tier SHOP plan average
monthly premiums age 21
Silver-tier SHOP plan average
monthly premiums age 40
Silver-tier SHOP plan average
monthly premiums age 60
State Low Median High Low Median High Low Median
High
Alabama $213 $262 $279 $272 $335 $357 $579 $711 $757
Alaska 480 491 523 613 627 669 1302 1332 1421
Arizona 165 217 449 211 278 574 448 590 1220
Arkansas
a
236 236 236 302 302 302 641 641 641
California 180 247 355 230 316 453 488 670 963
Colorado 251 296 382 321 378 489 681 804 1038
Connecticut 339 352 359 429 449 459 911 954 974
Delaware 277 293 303 354 374 388 753 795 823
District of Columbia 186 231 304 249 310 408 536 666 879
Florida 230 257 303 295 329 387 625 698 821
Georgia 214 252 316 273 322 404 580 684 857
Hawaii 138 192 208 176 245 266 375 521 565
Idaho 199 256 313 255 327 400 541 695 849
Illinois 203 295 335 259 377 428 550 802 909
Indiana 281 306 330 359 391 421 762 830 894
Iowa 185 272 356 236 347 455 502 738 966
Kansas 204 216 326 261 276 417 554 586 886
Kentucky 213 233 302 273 295 365 579 626 775
Louisiana 234 264 293 299 337 374 635 717 795
Maine 264 280 324 338 358 414 718 759 878
Maryland 183 271 354 233 346 453 495 735 961
Massachusetts 215 262 371 253 308 437 429 523 743
Michigan 151 280 346 193 358 442 410 761 939
Minnesota 193 251 309 247 321 400 524 681 861
Mississippi 243 246 264 310 314 337 658 667 715
Missouri
b
251 278 304 321 355 389 681 754 826
Montana 241 256 268 308 327 343 654 694 728
Nebraska 189 262 325 241 335 416 513 711 882
Nevada 199 226 356 255 289 456 541 614 967
New Hampshire
c
284 284 284 363 363 363 771 771 771
New Jersey 280 382 411 312 425 458 511 696 750
New Mexico 224 270 312 287 345 399 609 732 847
New York
d
North Carolina 309 317 323 395 405 413 838 859 878
Appendix III: Small Business Health Options
Program (SHOP) 2014 Average Monthly
Premiums for Silver-Tier Plans
Appendix III: Small Business Health Options
Program (SHOP) 2014 Average Monthly
Premiums for Silver-Tier Plans
Page 35 GAO-15-58 Small Business Health Insurance Exchanges
Silver-tier SHOP plan average
monthly premiums age 21
Silver-tier SHOP plan average
monthly premiums age 40
Silver-tier SHOP plan average
monthly premiums age 60
State
Low
Median
High
Low
Median
High
Low
Median
High
North Dakota 244 253 263 312 323 336 663 686 713
Ohio 228 278 330 292 355 421 620 755 895
Oklahoma 166 220 268 212 281 342 451 598 727
Oregon 197 283 347 252 361 443 535 768 941
Pennsylvania 186 240 306 238 306 391 506 651 830
Rhode Island 211 245 257 269 313 328 572 665 697
South Carolina 283 297 303 361 379 387 767 806 822
South Dakota 239 263 273 305 336 349 649 713 741
Tennessee 225 243 310 287 311 396 609 660 840
Texas 207 259 282 264 331 360 562 703 765
Utah 162 200 247 240 296 365 486 599 741
Vermont
e
395 422 429 395 422 429 395 422 429
Virginia 195 260 359 249 333 459 527 706 975
Washington 268 278 294 342 355 376 727 753 799
West Virginia
f
296 296 296 378 378 378 803 803 803
Wisconsin 224 282 450 286 361 576 608 766 1222
Wyoming 337 355 383 431 454 490 915 964 1040
Sources: GAO analysis of Centers for Medicare & Medicaid Services and state-based SHOP data. | GAO-15-58
Notes: All premiums have been rounded to the nearest dollar.
a
The Arkansas SHOP only had one plan available.
b
The Missouri SHOP only had two plans available.
c
The New Hampshire SHOP had only one plan available.
d
Premium data from New York was not available.
e
Vermont does not allow variation in plan premiums based on age.
f
The West Virginia SHOP had only one plan available.
Appendix IV: Small Business Health Options
Program (SHOP) Silver-Tier Plan Availability
Page 36 GAO-15-58 Small Business Health Insurance Exchanges
State
Total
silver-tier
plans
Issuers
offering
silver-tier
plans
Plans
available in
all counties
At least
two plans
in each
county
At least
two issuers
in each
county
Alabama 5 2 ● ● ●
Alaska 8 2 ● ● ●
Arizona 44 5 ● ● ●
Arkansas 1 1 ● ○ ○
California 11 6 ● ○ ○
Colorado 31 7 ● ● ●
Connecticut 3 3 ● ● ●
Delaware 4 2 ● ● ●
District of Columbia 89 7 ● ● ●
Florida 17 5 ● ○ ○
Georgia 7 3 ● ○ ○
Hawaii 13 2 ● ● ●
Idaho 17 3 ● ● ●
Illinois 20 3 ● ● ●
Indiana 58 2 ● ● ○
Iowa 28 5 ● ● ○
Kansas 3 2 ● ○ ○
Kentucky 8 4 ● ● ●
Louisiana 12 4 ● ● ●
Maine 4 2 ● ● ●
Maryland 29 13 ● ● ●
Massachusetts 19 10 ● ● ●
Michigan 21 8 ● ○ ○
Minnesota 22 3 ● ● ○
Mississippi 3 1 ● ● ○
Missouri 2 2 ● ○ ○
Montana 10 3 ● ● ●
Nebraska 14 4 ● ● ●
Nevada 6 2 ● ● ○
New Hampshire 1 1 ● ○ ○
New Jersey 11 3 ● ● ●
New Mexico 21 5 ● ● ●
New York
a
○ ○ ○
Appendix IV: Small Business Health Options
Program (SHOP) Silver-Tier Plan Availability
Appendix IV: Small Business Health Options
Program (SHOP) Silver-Tier Plan Availability
Page 37 GAO-15-58 Small Business Health Insurance Exchanges
State
Total
silver-tier
plans
Issuers
offering
silver-tier
plans
Plans
available in
all counties
At least
two plans
in each
county
At least
two issuers
in each
county
North Carolina 4 1 ● ● ○
North Dakota 6 3 ● ● ●
Ohio 39 6 ● ● ●
Oklahoma 22 3 ● ● ○
Oregon 28 8 ● ● ●
Pennsylvania 44 9 ● ● ○
Rhode Island 5 3 ● ● ●
South Carolina 5 3 ● ● ●
South Dakota 7 3 ● ● ●
Tennessee 4 2 ● ○ ○
Texas 9 2 ● ● ○
Utah 33 3 ● ● ●
Vermont 6 2 ● ● ●
Virginia 13 5 ● ○ ○
Washington 3 1 ○ ○ ○
West Virginia 1 1 ● ○ ○
Wisconsin 59 9 ○ ○ ○
Wyoming 5 2 ● ● ●
Legend: ● = Yes; ○ = No
Sources: GAO analysis of Centers for Medicare & Medicaid Services and state-based SHOP data. | GAO-15-58
a
Data on the total number of silver plans and the number of issuers offering silver plans was not
available for New York.
Appendix V: Comments from the Department
of Health and Human Services
Page 38 GAO-15-58 Small Business Health Insurance Exchanges
Appendix V: Comments from the Department
of Health and Human Services
Appendix V: Comments from the Department
of Health and Human Services
Page 39 GAO-15-58 Small Business Health Insurance Exchanges
Appendix VI: GAO Contact and Staff
Acknowledgments
Page 40 GAO-15-58 Small Business Health Insurance Exchanges
In addition to the contact name above, Randy DiRosa, Assistant Director;
Priyanka Sethi Bansal; Sandra George; Eagan Kemp; Laurie Pachter;
and Kate Tussey made key contributions to this report.
Appendix VI: GAO Contact and Staff
Acknowledgments
GAO Contact
Staff
Acknowledgments
(291189)
The Government Accountability Office, the audit, evaluation, and
investigative arm of Congress, exists to support Congress in meeting its
constitutional responsibilities and to help improve the performance and
accountability of the federal government for the American people. GAO
examines the use of public funds; evaluates federal programs and
policies; and provides analyses, recommendations, and other assistance
to help Congress make informed oversight, policy, and funding decisions.
GAO’s commitment to good government is reflected in its core values of
accountability, integrity, and reliability.
The fastest and easiest way to obtain copies of GAO documents at no
cost is through GAO’s website (http://www.gao.gov). Each weekday
afternoon, GAO posts on its website newly released reports, testimony,
and correspondence. To have GAO e-mail you a list of newly posted
products, go to http://www.gao.gov and select “E-mail Updates.”
The price of each GAO publication reflects GAO’s actual cost of
production and distribution and depends on the number of pages in the
publication and whether the publication is printed in color or black and
white. Pricing and ordering information is posted on GAO’s website,
http://www.gao.gov/ordering.htm.
Place orders by calling (202) 512-6000, toll free (866) 801-7077, or
TDD (202) 512-2537.
Orders may be paid for using American Express, Discover Card,
MasterCard, Visa, check, or money order. Call for additional information.
Connect with GAO on Facebook, Flickr, Twitter, and YouTube.
Subscribe to our RSS Feeds or E-mail Updates. Listen to our Podcasts.
Visit GAO on the web at www.gao.gov.
Contact:
Website: http://www.gao.gov/fraudnet/fraudnet.htm
E-mail: fraudnet@gao.gov
Automated answering system: (800) 424-5454 or (202) 512-7470
Katherine Siggerud, Managing Director, [email protected], (202) 512-
4400, U.S. Government Accountability Office, 441 G Street NW, Room
7125, Washington, DC 20548
Chuck Young, Managing Director, youngc1@gao.gov, (202) 512-4800
U.S. Government Accountability Office, 441 G Street NW, Room 7149
Washington, DC 20548
GAO’s Mission
Obtaining Copies of
GAO Reports and
Testimony
Order by Phone
Connect with GAO
To Report Fraud,
Waste, and Abuse in
Federal Programs
Congressional
Relations
Public Affairs
Please Print on Recycled Paper.
