Army Regulation 40–562
BUMEDINST 6230.15B
AFI 48–110_IP
CG COMDTINST M6230.4G
Medical Services
Immunizations and
Chemoprophylaxis
for the Prevention
of Infectious
Diseases
Headquarters
Departments of the Army,
the Navy,
the Air Force,
and the Coast Guard
Washington, DC
7 October 2013
UNCLASSIFIED
SUMMARY of CHANGE
AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G
Immunizations and Chemoprophylaxis for the Prevention of Infectious Diseases
This major revision, dated 7 October 2013--
o Changes the regulation title to "Immunizations and Chemoprophylaxis for the
Prevention of Infectious Diseases" (cover).
o Describes the responsibilities of the privileged physician with medical
oversight of any clinic or activity that administers immunizations (para 1-
4c(2)).
o Describes the responsibilities of the privileged health care provider, who is
under the direction of the privileged physician of any clinic or activity that
administers immunizations (para 1-4c(3)).
o Changes a reference to five-injection thresholds to reflect current evidence-
based practices (para 2-1e(1)).
o Adds a description of procedures for vaccine storage and handling (para 2-3).
o Adds a description of military indications for required and recommended
vaccines (paras 4-2 through 4-19).
o Makes changes to chemoprophylaxis recommendations (chap 5).
o Adds a description of procedures for documenting immunizations and
immunization recordkeeping (para B-5).
o Establishes and recommends immunization personnel training (para B-6 and
table B-1).
o Establishes criteria for determining required immunizations for military
personnel (app D).
o Makes administrative revisions (throughout).
Headquarters
Departments of the Army,
the Navy,
the Air Force,
and the Coast Guard
Washington, DC
7 October 2013
Medical Services
Immunizations and Chemoprophylaxis for the Prevention of Infectious Diseases
*Army Regulation 40–562
*BUMEDINST 6230.15B
*AFI 48–110_IP
*CG COMDTINST M6230.
4G
Effective 7 November 2013
H i s t o r y . T h i s p u b l i c a t i o n i s a m a j o r
revision.
Summary. This regulation for immuni-
z a t i o n a n d c h e m o p r o p h y l a x i s u p d a t e s
quality standards for immunization deliv-
e r y ; e s t a b l i s h e s e l e c t r o n i c i m m u n i z a t i o n
tracking systems as the preferred immuni-
zation record; provides guidance for lost
i m m u n i z a t i o n r e c o r d s , i m m u n i z a t i o n
c r e d i t f o r p r e - e x i s t i n g i m m u n i t y , a n d
complying with regulations for vaccines
and other products administered in inves-
tigational, new drug status or in accord-
a n c e w i t h e m e r g e n c y u s e a u t h o r i z a t i o n ;
describes dividing initial entry immuniza-
tion into two clusters; and describes the
role of the Military Vaccine Office.
Applicability. This regulation applies to
t h e A c t i v e A r m y , t h e A r m y N a t i o n a l
Guard/Army National Guard of the United
States, and the U.S. Army Reserve, unless
otherwise stated. It also applies to the fol-
l o w i n g : u n i f o r m e d D e p a r t m e n t s o f t h e
Navy, Air Force, and Coast Guard (in-
cluding the active and reserve components
o f e a c h S e r v i c e ) ; n o n m i l i t a r y p e r s o n s
under military jurisdiction; selected Fed-
e r a l e m p l o y e e s ; s e l e c t e d e m p l o y e e s o f
Department of Defense contractors; and
F a m i l y m e m b e r s a n d o t h e r h e a l t h c a r e
beneficiaries eligible for care within the
military health care system. This regula-
tion is applicable during mobilization.
Proponent and exception authority.
The proponent of this regulation is The
Surgeon General. The proponent has the
authority to approve exceptions or waivers
to this regulation that are consistent with
controlling law and regulations. The pro-
ponent may delegate this approval author-
ity, in writing, to a division chief within
the proponent agency or its direct report-
ing unit or field operating agency, in the
grade of colonel or the civilian equivalent.
Activities may request a waiver to this
regulation by providing justification that
includes a full analysis of the expected
benefits and must include formal review
by the activity’s senior legal officer. All
waiver requests will be endorsed by the
commander or senior leader of the requ-
e s t i n g a c t i v i t y a n d f o r w a r d e d t h r o u g h
t h e i r h i g h e r h e a d q u a r t e r s t o t h e p o l i c y
proponent. Refer to AR 25–30 for specific
guidance.
Army internal control process. This
regulation contains internal control provi-
sions and identifies key internal controls
that must be evaluated (see appendix E).
S u p p l e m e n t a t i o n . S u p p l e m e n t a t i o n o f
this regulation and establishment of com-
mand and local forms are prohibited with-
o u t p r i o r a p p r o v a l f r o m T h e S u r g e o n
G e n e r a l ( D A S G – Z A ) , 7 7 0 0 A r l i n g t o n
Blvd., Falls Church, VA 22041–5143.
Suggested improvements. Users are
invited to send comments and suggested
improvements on DA Form 2028 (Recom-
m e n d e d C h a n g e s t o P u b l i c a t i o n s a n d
B l a n k F o r m s ) d i r e c t l y t o T h e S u r g e o n
G e n e r a l ( D A S G – Z A ) , 7 7 0 0 A r l i n g t o n
Blvd., Falls Church, VA 22041–5143. Air
Force users are invited to send comments
and suggested improvements on AF Form
8 4 7 ( R e c o m m e n d a t i o n s f o r C h a n g e o f
P u b l i c a t i o n ) t h r o u g h c h a n n e l s t o H e a d -
quarters, AFMSA/SGOP, 7700 Arlington
Blvd., Falls Church, VA 22041–5143.
Distribution. This publication is availa-
ble in electronic media only and is in-
tended for command levels A, B, C, D,
and E for the Active Army, the Army
National Guard/Army National Guard of
the United States, and the U.S. Army Re-
serve. Navy/Marine Corps: Ships, units,
a n d s t a t i o n s h a v i n g m e d i c a l d e p a r t m e n t
personnel. Air Force: Active Air Force,
the Air National Guard, and Air Force
R e s e r v e . C o a s t G u a r d : A c t i v e C o a s t
Guard and Coast Reserves.
*This regulation supercedes AR 40–562/BUMEDINST 6230.15A/AFJI 48–110/CG COMDTINST M6230.4F, dated 29 September 2006.
AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013 i
UNCLASSIFIED
Contents (Listed by paragraph and page number)
Chapter 1
Introduction, page 1
Purpose • 1–1, page 1
References • 1–2, page 1
Explanation of abbreviations and terms • 1–3, page 1
Responsibilities • 1–4, page 1
Chapter 2
Program Elements and Clinical Considerations, page 2
Standards • 2–1, page 2
Logistics • 2–2, page 3
Storage and handling • 2–3, page 3
Hypersensitivity or allergy • 2–4, page 5
Immunizing women of childbearing potential • 2–5, page 5
Exemptions • 2–6, page 6
Immunization and chemoprophylaxis records • 2–7, page 7
Jet-injection immunization devices • 2–8, page 8
Emergency response requirements • 2–9, page 8
Adverse events • 2–10, page 9
Program evaluation • 2–11, page 9
Blood donation • 2–12, page 10
Chapter 3
Personnel Subject to Immunization, page 10
Military accessions • 3–1, page 10
Military personnel • 3–2, page 11
Certain civilian employees • 3–3, page 11
Contracted workers • 3–4, page 12
Department of Defense, U.S. Coast Guard schools, childcare centers and youth programs • 3–5, page 12
Other populations • 3–6, page 13
Chapter 4
Specific Immunization Requirements for Department of Defense and U.S. Coast Guard Personnel,
page 13
Civilian applicability • 4–1, page 13
Adenovirus types 4 and 7 • 4–2, page 13
Anthrax • 4–3, page 13
Haemophilus influenzae serotype b, commonly called Hib • 4–4, page 14
Hepatitis A • 4–5, page 14
Hepatitis B • 4–6, page 14
Influenza • 4–7, page 14
Japanese encephalitis • 4–8, page 14
Measles, mumps, and rubella (MMR) • 4–9, page 15
Meningococcal • 4–10, page 15
Pertussis • 4–11, page 15
Pneumococcal • 4–12, page 15
Poliomyelitis • 4–13, page 15
Rabies • 4–14, page 16
Smallpox • 4–15, page 16
Tetanus, diphtheria, and pertussis • 4–16, page 16
Typhoid fever • 4–17, page 17
Varicella • 4–18, page 17
ii AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Contents—Continued
Yellow fever • 4–19, page 17
Chapter 5
Chemoprophylaxis, page 18
General • 5–1, page 18
Anthrax • 5–2, page 18
Group A streptococcus • 5–3, page 18
Influenza • 5–4, page 18
Leptospirosis • 5–5, page 19
Malaria • 5–6, page 19
Meningococcal disease • 5–7, page 19
Plague • 5–8, page 19
Scrub typhus • 5–9, page 19
Smallpox • 5–10, page 19
Traveler’s diarrhea • 5–11, page 19
Chapter 6
Biological Warfare Defense, page 20
Responsibilities • 6–1, page 20
Procedures • 6–2, page 20
Chapter 7
Vaccines and Other Products in Investigational New Drug Status, page 20
Purpose • 7–1, page 20
General guidance on investigational new drug products • 7–2, page 20
Health recordkeeping requirements for investigational new drug products • 7–3, page 20
Information requirements for investigational new drug products • 7–4, page 21
Coordination • 7–5, page 21
Chapter 8
Vaccines and Other Products Used Under Emergency Use Authorization, page 21
General • 8–1, page 21
Criteria • 8–2, page 21
Refusal options • 8–3, page 21
Health recordkeeping requirements for emergency use authorization products • 8–4, page 21
Information requirements for emergency use authorization products • 8–5, page 21
Department of Defense requests for emergency use authorizations • 8–6, page 21
Coordination • 8–7, page 21
Appendixes
A. References, page 22
B. Standards for Military Immunization, page 25
C. Medical and Administrative Exemption Codes, page 28
D. Immunizations for Military Personnel, page 29
E. Internal Control Evaluation Process, page 30
Table List
Table B–1: Training standards, page 26
Table C–1: Medical exemption codes, page 28
Table C–2: Administrative exemption codes, page 28
Table D–1: Immunizations for military personnel, page 29
Glossary
iiiAR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Chapter 1
Introduction
1–1. Purpose
This publication provides directive requirements for the Military Vaccination Program; establishes general principles,
procedures, policies, and responsibilities for the immunization program; and implements military and international
health regulations and requirements.
1–2. References
Required and related publications and prescribed and referenced forms are listed in appendix A.
1–3. Explanation of abbreviations and terms
Abbreviations and special terms used in this regulation are explained in the glossary.
1–4. Responsibilities
a . C o m m a n d m e d i c a l a u t h o r i t y . T h e c o m m a n d m e d i c a l a u t h o r i t y w i l l p r e s c r i b e s p e c i f i c i m m u n i z a t i o n a n d
chemoprophylactic requirements for their units per requirements established by this publication and additional guidance
provided by the appropriate surgeon general or the U.S Coast Guard (USCG), Director of Health, Safety, and Work-
Life (USCG, CG–11).
b. Command leaders. Combatant commanders, major command commanders, unit commanding officers, command-
ers of special operations and forces, and officers-in-charge will:
( 1 ) E n s u r e m i l i t a r y a n d n o n m i l i t a r y p e r s o n n e l u n d e r t h e i r j u r i s d i c t i o n r e c e i v e r e q u i r e d i m m u n i z a t i o n s a n d
chemoprophylaxis. Ensure immunizations and immunization exemption codes (medical or administrative) are docu-
mented in an approved Department of Defense (DOD) or USCG Service Immunization Tracking System (ITS), as
described in paragraph 2–7a.
(2) Maintain appropriate international, Federal, State, and local records of all immunizations and chemoprophylaxis.
(3) Ensure personnel transferred to another command or unit, including advanced instructional training or technical
school, receive proper screening for, and administration of, appropriate immunizations and chemoprophylaxis for the
area assigned, and are timed to provide immunity before deployment or exposure or to complete a vaccine series.
(4) Ensure immunization exemptions are documented in the Service ITS.
(5) Ensure vaccine doses or boosters are administered to complete a started series or maintain immunity.
(6) Ensure deviations from specified immunizations are cleared or authorized by the appropriate combatant com-
mander; surgeon general; or USCG, CG–11.
(7) Observe international military standardization agreements (STANAGs).
c. Medical commanders, commanding officers, and command surgeons. Medical commanders, commanding officers,
and command surgeons will:
(1) Ensure individuals administering immunizations are properly trained in accordance with DOD, Service, and
Centers for Disease Control and Prevention (CDC) guidelines and act within their scope of practice as determined by
each Service. A training checklist is found in appendix B, paragraph B–6 and table B–1.
(2) Appoint, in writing, a privileged physician with medical oversight over any clinic or activity that administers
immunizations. This physician will:
(a) Complete appropriate training in immunization science in residence or via distance learning.
(b) Be available to address immunization issues, although it is not required that the privileged physician be present
for administration of vaccines. The USCG requires a privileged health care provider to administer immunizations to
civilians who are eligible for care in a medical treatment facility.
(c) Establish and sign vaccine and chemoprophylaxis standing orders for clinics or other locations where immuniza-
tions or chemoprophylaxis medications are administered.
(d) Ensure standard operating procedures (SOPs) are established that implement current national standards for adult
and pediatric immunizations and chemoprophylactic practices and promote appropriate quality improvement mecha-
nisms. Incorporate local practices and requirements of policies contained in references listed at appendix A.
(3) Appoint, in writing, a privileged health care provider, who is under the direction of the privileged physician
appointed in paragraph 1–4c(2), to have oversight over the daily activities of any clinic or activity that administers
immunizations. The privileged physician may serve as the health care provider if no one is available to assume the
position of privileged health care provider.
(4) Ensure patients are evaluated for preexisting immunity, screened for administrative and medical exemptions,
and/or evaluated for the need for medical exemptions to immunizations or chemoprophylaxis medications. Exemptions
are granted per paragraph 2–6; document any exemptions.
(5) Monitor the immunization status of personnel and ensure compliance with policies and procedures for creating
and maintaining immunization records in accordance with Title 42, United States Code, Chapter 300aa-25.
(6) Ensure emergency medical response is available and that personnel who administer immunizations receive
1AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
training on: basic cardiopulmonary resuscitation, administration of epinephrine, and emergency response to immuniza-
tion-adverse events, at a minimum.
(7) Ensure health care providers are available to respond to and report adverse events resulting from immunization.
(8) Ensure patients needing evaluation of adverse events after immunization are referred to appropriate health care
providers, such as medical subspecialists (including specialists in immunization health care) for evaluation, consulta-
tion, or indicated intervention.
d. The Army, as Executive Agent for the Military Vaccination Program. The Army, as Executive Agent for the
Military Vaccination Program and in cooperation with the Military Services, will:
(1) Operate a Military Vaccine (MILVAX) Office to provide the Military Services with a coordinated source for
information and education of vaccine-related activities needed in order to implement Department of Defense Directive
(DODD) 6205.3, DODD 6205.02E, and Department of Defense Instruction (DODI) 6205.4.
(2) Synchronize, integrate, and coordinate immunization policies and other immunization-related activities for all
DOD components.
(3) Facilitate and promote the quality of immunization policy, implementation, education, distribution, risk commu-
nication, administration, clinical services, safety surveillance, research, and program evaluation.
(4) Provide a comprehensive access point to provide information, education resources, safety surveillance, and
uniform procedures to identify, report, and evaluate vaccine-associated adverse events.
(5) Maintain historical vaccine usage data as well as identify future vaccine requirements as needed.
(6) Provide primary coordination between DOD and vaccine manufacturers for all applicable post-licensure vaccine
studies.
(7) Coordinate with other Secretaries of the Military Departments and the Commandant, USCG to:
(a) Establish joint clinical quality standards for immunization delivery and education and training to personnel
involved in immunization healthcare. The goals of these standards are to promote clinical excellence and decrease
practice variability.
(b) Assess the DOD Immunization Program by developing metrics to measure individual medical readiness, vaccine
effectiveness and safety, and compliance with overall immunization policies.
(c) Regularly update the Joint Regulation on Immunization and Chemoprophylaxis for the Prevention of Infectious
Diseases.
(8) Promote scholarly immunization study activities through the Army’s Medical Infectious Disease Research
Program using funds both from the Defense Health Program and the Research, Development, Test, and Evaluation.
e. Each of the Military Services. Each of the Military Services will provide an immunization health care capability
to deliver medical specialty consultation, case management, and clinical investigation. The U.S. Navy provides medical
services for the U.S. Marine Corps.
Chapter 2
Program Elements and Clinical Considerations
2–1. Standards
a. Department of Defense and U.S. Coast Guard policy. The Military Service policy concerning immunizations
follows the recommendations of the CDC and the Advisory Committee on Immunization Practices (ACIP) and the
prescribing information on the manufacturer’s package inserts, unless there is a military-relevant reason to do other-
wise. Any vaccine or drug licensed by the U.S. Food and Drug Administration (FDA) or the U.S. Department of
Health and Human Services (DHHS) may be used, as well as vaccines or drugs compliant with applicable DOD
investigational new drug (IND) or emergency use authorization (EUA) processes. Privileged health care providers may
make clinical decisions for individual beneficiaries to customize medical care or to respond to an individual clinical
situation that is compliant with IND or EUA processes.
b. Standards for delivery of military vaccines. Standards for delivery of military vaccines are provided in appendix
B. Military Services will abide by these standards in routine immunization delivery.
c. Expiration date. Vaccines or drugs will not be used beyond the manufacturer’s potency expiration date, unless the
appropriate surgeon general or USCG, CG–11, authorizes extension in exceptional circumstances.
d. Screening for contraindications. Screen all potential vaccines for contraindications, precautions, or warnings per
the prescribing information on the manufacturer’s package insert.
e. Immunization schedules and intervals.
(1) Initial series. Once an immunization series has been started, it must be completed, unless a medical or
administrative exemption exists. Restarting an immunization series or adding extra doses is not necessary when an
initial series of a vaccine or toxoid is interrupted; instead, give delayed doses as soon as feasible.
(2) Doses. Vaccine doses in an initial series will not be administered at intervals less than the recommended
minimum intervals or earlier than the minimum age unless the doses are part of a CDC catch-up schedule or during an
2 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
outbreak. Doses in an initial series administered 5 or more days earlier than the minimum interval should not be
counted as valid doses. The next valid dose is calculated after the last invalid dose.
(3) Booster doses. After the initial series of a vaccine is complete, a booster dose may be recommended for specific
vaccines. For vaccines that do not provide lifetime immunity, the booster dose is usually recommended or required to
increase immunity back to protective levels.
f. Simultaneous immunizations.
(1) When simultaneous vaccine injections are necessary, administer vaccines in different limbs. The anatomical site
may depend on the age of the individual, and the degree of muscle development. If different anatomical sites are not
possible, then separate the injections by at least 1 inch. Refer to the ACIP General Recommendations on Immuniza-
tions for proper needle lengths.
(2) Priority of immunization is based on the relative likelihood of various microbial threats and the existence of any
vaccine-vaccine, vaccine-antibody, or vaccine-drug interactions and is best performed by the health care provider. In
military training centers, contagious diseases typically represent the most imminent threats.
(3) Spacing of live and inactivated vaccines.
(a) Two or more inactivated vaccines can be administered simultaneously or at the prescribed interval and restric-
tions indicated in the package insert for each vaccine.
(b) Inactivated and live vaccines can be administered simultaneously or at the prescribed interval and restrictions
indicated in the package insert for each vaccine.
(c) Two or more live virus vaccines must be administered simultaneously or separated by at least 28 days (4 weeks).
Refer to ACIP guidelines for exceptions.
g. Screening for immunity. For some vaccine-preventable diseases, serologic or other tests can be used to identify
pre-existing immunity from prior infections or immunizations that may eliminate unnecessary immunizations.
h. Live virus vaccines and tuberculosis testing. Vaccinations with live vaccines may affect tuberculosis (TB) testing.
This includes both the Mantoux tuberculin skin test and the Intereferon-Gamma Release Assays test whole-blood test.
To avoid interference:
(1) Administer live virus vaccines and TB test on the same day.
(2) Perform TB test 4 to 6 weeks after administration of live virus vaccines, or
(3) Administer live virus vaccines, once the TB test is read.
2–2. Logistics
a. Requisitioning of immunizing and chemoprophylaxis agents. Immunizing and chemoprophylaxis agents are requi-
sitioned in accordance with medical supply procedures. However, vaccinia immune globulin—also known as VIG-
intravenous—is available only by ordering through the MILVAX Office.
b. Transportation, storage, and handling. All personnel will maintain the cold chain in vaccine delivery during
transportation, storage, and handling. Shipping and storage advice is available from Services medical logistics centers.
c. Small stations, ships, and cutters. To minimize the shipment of vaccines that must be stored at frozen tempera-
tures, small stations, ships, and cutters may requisition these items from a nearby military medical activity stocking the
items. Requisitioning procedures and reimbursement are prescribed by the supplying activity.
2–3. Storage and handling
a. Safety and efficacy of vaccines. Failure to adhere to recommended specifications for storage and handling of
vaccines may reduce potency, resulting in inadequate immune responses in the recipients and inadequate protection
against disease. To maintain the safety and efficacy of vaccines, ensure immunizing and chemoprophylaxis agents are
stored, shipped, and handled in accordance with the pharmaceutical manufacturer’s instructions as outlined in the
product package insert or other guidance.
b. Policies for maintaining vaccines. All locations that maintain and administer vaccines will develop and imple-
ment policies and procedures for maintaining cold chain management of vaccines.
c. Shelf-life after opening.
(1) Administer vaccines shortly after withdrawal from single-dose or multi-dose vials, in accordance with the
manufacturer’s package insert.
(2) Single dose vials are meant for one-time use only. At the end of the clinic day, discard all single-dose vials
without protective caps.
(3) For multi-dose vaccine vials that do not require reconstitution, doses that remain after withdrawal of a dose can
be administered until the expiration date printed on the vial or vaccine packaging, so long as the vial has been stored
correctly and the vaccine is not visibly contaminated and the manufacturer has not specified otherwise.
(4) Multi-dose vials that require reconstitution must be used within the interval specified by the manufacturer. After
reconstitution, the new expiration date should be written on the vial.
d. Diluents.
(1) Diluents are not interchangeable, unless specified by the manufacturer.
3AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
(2) Transport diluents at room temperature in validated containers, but not in direct contact with shipping gel packs.
(3) Store diluents according to the manufacturer’s package insert.
(4) Discard diluents when stored inappropriately or expired.
e. Filling syringes and attaching needles.
(1) Never mix individual vaccines in the same syringe. Different vaccines should never be mixed in the same
syringe unless specifically licensed for such use. Do not transfer vaccine between syringes.
(2) Use a separate needle and syringe for each injection.
(3) Label filled syringes with the type of vaccine, lot number, and date of filling, unless the vaccine is administered
immediately after being drawn into the syringe by the same person administering the vaccine.
(4) Attach needles to manufactured filled syringes just prior to administration. Discard needle and syringe if the
vaccine is not administered before the end of the clinic day or vaccination session in accordance with the manufactur-
er’s package insert. If no time line is provided, discard after 8 hours.
f. Prefilling syringes.
(1) Prefilling syringes is highly discouraged because of the increased risk of administration errors and possible
bacterial growth in vaccines that do not contain preservatives. Syringes other than those filled by the manufacturer are
designed for immediate use and not for vaccine storage.
(2) In certain circumstances in which a single vaccine type is being used, such as during an influenza vaccination
campaign, filling a small number of syringes may be considered.
(3) Discard unused syringes filled by the end user (that is, not filled by the manufacturer) in accordance with the
manufacturer’s package insert. If no time line is provided, discard after 8 hours.
g. Storing vaccine.
(1) Ensure that only vaccines are stored in the vaccine storage unit (refrigerator or freezer).
(2) Store refrigerated vaccines at temperatures of 35°F to 46°F (2°C to 8°C). Do not expose refrigerated vaccines to
freezing temperatures.
(3) Store frozen vaccines at temperatures of 5°F (-15°C) or lower.
(4) Store all reconstituted lyophilized (freeze-dried) vaccines in accordance with the manufacturer’s temperature and
light condition parameters.
h. Vaccine storage equipment. Ensure that vaccine storage units are carefully selected, used properly, and consis-
tently monitored to maintain recommended vaccine storage temperatures.
(1) Stand-alone refrigerators and freezers are recommended for storage of vaccines. A combination refrigerator/frost-
free freezer for home use is acceptable if only the refrigerator compartment of the combination unit is used to store
refrigerated vaccines. A separate stand-alone freezer should then be used to store frozen vaccine. Dormitory style
refrigerators are not authorized for vaccine storage.
(2) Use certified and calibrated thermometers in all vaccine storage units. Uncertified liquid (mercury or alcohol)
thermometers and uncertified dial-type household refrigerator/freezer thermometers are not authorized.
(3) Ensure alarm systems are incorporated as part of the vaccine storage unit to alert staff of power failures or
indicate whether or not vaccine temperatures have been maintained.
i. Temperature tracking.
(1) Ensure temperatures are documented for each vaccine storage unit. Physically confirm the temperature of all
vaccine refrigerators and freezers at a minimum of two times per day. Document the date, time, and temperature of the
vaccine storage unit on a temperature log. Vaccine outside of a refrigerator or freezer must have the temperature
checked and documented every hour.
(2) Keep temperature logs for at least 3 years. State and/or local requirements may require longer recordkeeping.
(3) Record date and time of any mechanical malfunction or power outage on the temperature log or on another
equipment-tracking document.
j. Vaccine storage alarms.
(1) Ensure alarm systems are capable of monitoring vaccine storage 24 hours a day, 7 days per week. Ensure the
system either notifies an accountable person when a failure is detected, or the system is capable of indicating that the
vaccine temperature integrity was maintained during the storage period (or notes any deviations).
(2) Ensure current personnel contact information exists on auto-dialers, and that appropriate coverage occurs during
periods of leave, holiday weekends, and so forth.
(3) Monitor alarms electronically and physically 24 hours a day, 7 days per week.
(4) Test the entire alarm system, to include refrigerator-freezer-unit sensor to the remote monitoring station and
telephone or pager, at least monthly. Maintain test records for at least 3 years.
(5) For vaccine storage units within restricted access areas, ensure the temperature can be checked and a light or
audible alarm is installed to indicate when the storage unit temperature is out of range without having to physically
enter the restricted area.
k. Transporting vaccines.
4 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
(1) Always transport vaccines in properly insulated containers to maintain the recommended temperatures.
(2) Ensure containers used for transporting vaccines are capable of maintaining the vaccine at the correct tempera-
tures. Validated storage devices include the Vaxicool, Vaxipac, manufacturer shipping containers, Styrofoam(tm)
coolers with at least 2-inch thick walls, or Endurotherm insulating shipping containers.
(3) Pack containers to appropriately maintain the proper temperature while vaccine is transported or shipped.
Refrigerated or frozen packs are authorized for use to maintain the cold chain when used according to the U.S. Army
Medical and Materiel Agency (USAMMA) Distribution Operations Center instructions.
(4) Include calibrated thermometers to track temperatures in all transportation and off-site storage containers.
(5) Pack vaccines in their original packaging. Do not remove vaccine vials from boxes.
(6) Document vaccine type, quantity, date, time, and originating facility on the outside of the transportation
containers.
(7) Ensure temperatures are tracked during transportation and any deviations in temperature are readily identifiable.
l. Vaccine disposal or disposition.
(1) Discard syringes or vials that contain live virus vaccines per installation policy.
(2) Contact the pharmacy or logistics office for specific policies regarding the disposition of unopened vials, expired
vials, unused doses, and potentially compromised vaccine.
(3) Label potentially compromised vaccines with the words “Do not use” and place in the refrigerator or freezer
based on the manufacturer’s instructions as if they were not compromised. Report all compromised anthrax, smallpox,
and influenza vaccines to USAMMA for validation before destruction. Contact the manufacturer for all other poten-
tially compromised vaccines for disposition or destruction instructions.
(4) Report all confirmed compromised vaccine losses through Service-specific channels to the Military Vaccine
Office. The report must include the following: description of the reason for the loss, vaccines compromised, total vials/
doses lost, and cost of lost or compromised vaccines.
2–4. Hypersensitivity or allergy
a. Before administration of any medication, including vaccines, determine if the individual has previously shown
any unusual degree of adverse reaction or allergy to it or any specific component of the vaccine or its packaging (for
example, eggs, gelatin, preservatives, latex). Review the manufacturers’ package inserts and reference materials for
product-specific information.
b. Defer individuals with reported hypersensitivity to a particular vaccine or its components from immunization.
c. Refer individuals with a hypersensitivity to an appropriate medical specialist for evaluation, unless the health
record contains documentation of a prior consultation or a specialist’s recommendations. Document hypersensitivity
and any recommended exemption(s) in the electronic ITS and the appropriate sections of the health record.
2–5. Immunizing women of childbearing potential
A pregnancy screening test for women of childbearing potential is not routinely required before administering vaccines,
including live virus vaccines. Take the following precautions to avoid unintentional immunization with contraindicated
products during pregnancy—
a. Display signs asking pregnant women to identify themselves. Discreetly ask her if she is, or might be, pregnant.
Document responses in the health record. If the answer is “yes,” and the ACIP does not recommend the vaccine for use
in pregnancy, then defer her from immunization or refer to an obstetric healthcare provider to determine whether the
benefits of immunization outweigh risks in pregnancy. If the vaccine is recommend for use in pregnancy by ACIP, the
vaccine may be administered. If pregnancy status is uncertain, defer immunization until after a negative pregnancy
evaluation (for example, urine, or serologic test).
b. With regard to smallpox (vaccinia) vaccine, a specific pre-immunization screening form (available at http://www.
smallpox.mil/resource/forms.asp) that assesses the date of the last menstrual period is required. For women whose last
menstrual period was more than 28 days ago, a pregnancy test is recommended.
c. Breastfeeding women may be immunized in accordance with the current ACIP guidelines. At present, no
immunization products are medically contraindicated in breastfeeding women. Smallpox vaccine is withheld from
breastfeeding women, except in an outbreak, primarily due to the potential for contact transmission of vaccinia virus to
the child.
d. If a live virus vaccine is administered, counsel her to avoid becoming pregnant for the appropriate interval as
recommended by CDC or the vaccine manufacturer. Document the counseling in the health record.
e. If she is pregnant and immunization is indicated, immunize in consultation with her obstetric health care provider.
f. If a contraindicated vaccine is inadvertently administered to a pregnant woman, report the event upon discovery to
the preventive medicine point of contact and obstetric services and complete appropriate quality assurance documents.
Report such cases to any applicable registry. For assistance with registry referral procedures, contact the preventive
medicine service or MILVAX.
5AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
2–6. Exemptions
There are two types of exemptions from immunization-medical and administrative. Granting medical exemptions is a
medical function. Granting administrative exemptions is a nonmedical function.
a. Medical exemptions. A medical exemption includes any medical contraindication relevant to a specific vaccine or
other medication. Health care providers will determine a medical exemption based on the health of the vaccine
candidate and the nature of the immunization under consideration. Medical exemptions may be temporary (up to 365
days) or permanent. Standard exemption codes appear in appendix C.
(1) General examples of medical exemptions include the following—
(a) Underlying health condition of the vaccine candidate (for example, based on immune competence, phar-
macologic or radiation therapy, pregnancy and/or previous adverse response to immunization).
(b) Evidence of immunity based on serologic tests, documented infection, or similar circumstances.
(c) An individual’s clinical case is not readily definable. In such cases, consult appropriate medical specialists,
including specialists in immunization health care.
(2) Providers who are assessing medical exemptions may seek a second opinion from a provider experienced in
vaccine adverse event management, such as specialists in immunization health care at a medical center, or seek
additional consultation from MILVAX.
(3) Annotate electronic ITS and paper-based service treatment records with exemption codes denoting evidence of
immunity, severe adverse event after immunization (except for the Medical Readiness Reporting System), other
temporary or permanent reasons for medical exemption, and other appropriate categories.
(4) Report cases warranting permanent medical exemptions due to a vaccine related adverse event to the Vaccine
Adverse Events Reporting System (VAERS) at the Web site at http://www.vaers.hhs.gov and as discussed in paragraph
2–10.
(5) Revoke medical exemptions when they are no longer clinically warranted.
b. Administrative exemptions. Standard exemption codes appear in appendix C.
(1) Separation or retirement. Within 180 days before separation or retirement, Service personnel may be exempt
from deployment (mobility) immunizations, if one of the following conditions are met:
(a) They are not currently assigned, deployed, or scheduled to perform duties in a geographical area where an
immunization is indicated.
(b) The commander has not directed immunization because of overriding mission requirements. Personnel who meet
separation or retirement requirements and desire an immunization exemption must identify themselves to their com-
mander. The member must have approved retirement or separation orders. Active duty personnel continuing duty in the
reserve component are not exempted on this basis.
(2) Thirty days or fewer of service remaining. Applies to civilian employees and contractor personnel who will leave
a permanent (other than OCONUS deployments) assignment subject to immunization within 30 days or fewer.
(3) Religious exemptions.
(a) Servicemembers. Immunization exemptions for religious reasons may be granted according to Service-specific
policies to accommodate religious beliefs of a Service member. This is a command decision made with medical, judge
advocate, and chaplain input.
1. Requests for religious exemption must comply with the provisions of the applicable policy and/or regulation for
the Servicemember requesting religious accommodation. For the Army, religious accommodation policy is provided in
AR 600–20. For the Navy and Marine Corps, waivers are granted on a case-by-case basis by the Chief, Bureau of
Medicine, and Surgery. For the Air Force, permanent exemptions for religious reasons are not granted; the MAJCOM
commander is the designated approval and revocation authority for temporary immunization exemptions. For the Coast
Guard, CG–122 is the designated approval and revocation authority for religious immunization exemptions. USCG
requests must be forwarded through the appropriate chain to Commandant CG–122 via CG–112.
2. A military physician must counsel the applicant. The physician should ensure that the Servicemember is making
an informed decision and should address, at a minimum, specific information about the diseases concerned; specific
vaccine information including product constituents, benefits, and risks; and potential risks of infection incurred by
unimmunized individuals.
3. The commander must counsel the individual that noncompliance with immunization requirements may adversely
impact deployability, assignment, or international travel.
4. Per DODI 1300.17 and applicable service regulations will be provided whether Servicemembers with pending
active requests for religious exemption are temporarily deferred from immunizations, pending outcome of their request.
5. Religious exemptions may be revoked, in accordance with Service-specific policies and procedures, if the
individual and/or unit are at imminent risk of exposure to a disease for which an immunization is available.
(b) Civilian employees. Civilian employees submit requests for immunization exemption for religious reasons to
their supervisors. Civilian requests are processed in accordance with Part 1605, Title 29, Code of Federal Regulations
and component policies.
(c) Bargaining units. Civilian personnel affected by this document who are members of bargaining units will be
6 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
considered for exemption consistent with applicable personnel management policies and applicable labor relations
obligations.
(d) Other exemption categories. Administrative or medical personnel will appropriately annotate electronic ITS with
exemption codes denoting separation, permanent change of station, emergency leave, missing or prisoner of war,
deceased, and other appropriate categories.
2–7. Immunization and chemoprophylaxis records
a. Electronic immunization tracking systems.
(1) Document all immunizations in a DOD and USCG-approved ITS. Include date, immunization given, dose,
anatomical location of administration, lot number, manufacturer, Vaccine Information Sheet (VIS) date, and the
identification of the person administering the vaccine.
(2) Electronic ITS must—
(a) Comply with the requirements of the National Vaccine Injury Compensation (NVIC) Program as provided in 42
USC 300aa-25, Report and Recording of Information, and 42 USC 300aa-26. NVIC information is outlined in
paragraph 2–7d.
(b) Incorporate DOD-directed levels of security, certification, and redundancy, and the requirements of the Health
Insurance Portability and Accountability Act to preclude unauthorized access to personal medical information and to
survive hardware or software malfunction.
(c) Be capable of generating printed reports of immunization status and exemption information on both an individual
and unit basis.
(3) A printed report from the electronic ITS, in CDC Form 731 (International Certificate of Vaccination or
Prophylaxis) 731, SF 601 (Health Record-Immunization Record), or DD Form 2766C (Adult Preventive and Chronic
Care Flowsheet) (Continuation Sheet) format, accompanied by an official clinic stamp and the authorized signature and
printed name of an authenticating official, will qualify as an official paper immunization record.
(4) A printed report as identified in preceding paragraph 2–7a(3) will suffice as a valid certificate of vaccination for
international travel (except for yellow fever which is documented on the CDC Form 731) for active duty members of
the Armed Forces as outlined in Article 36 (Annex 6) of the World Health Organization (WHO) International Health
Regulations.
b. Non-electronic immunization and chemoprophylaxis records.
(1) Deployment records. Transfer information regarding immunizations and chemoprophylaxis including date, prod-
uct given, dose, and initials of person administering to the deployable health record (DD Form 2766) or comparable
approved form, either by computer-generated report or by hand. Upon return from deployment, transfer entries on the
deployment record into the appropriate ITS or other electronic record system.
(2) Abbreviations. Use abbreviations for vaccines and their manufacturers conforming to the nomenclature adopted
by the CDC Vaccine Identification Standards Initiative. When annotating the date a vaccine is administered, the day,
month, and year are listed in that order. The day is expressed in Arabic numerals, the month spelled out or abbreviated
using the first three letters of the word, and the year expressed in Arabic numerals either by four digits or by the last
two digits (for example, 14 June 1994 or 14 Jun 94).
(3) Transcribed records. Entries based on prior official records will include the following statement: “Transcribed
from official records.” Alternately, the statement may cite the specific source (for example, “Transcribed from SF
601”). When entries are transcribed onto paper records, include the initials of the transcriber on each entry.
(4) SF 601 (Navy, Marine Corps, and U.S. Coast Guard). Prepare SF 601 in accordance with this directive and
chapter 16 of NAVMED P–117.
(5) DD Form 2766C. Initiate DD Form 2766C for all personnel at the time of entry into Military Service.
(6) Paper-based immunization and chemoprophylaxis records. Individuals preparing paper-based immunization and
chemoprophylaxis records will ensure that paper records match the electronic ITS. If paper-based immunization or
chemoprophylaxis records are used, electronic ITS will be updated within 24 hours.
(7) CDC Form 731. Required for yellow fever documentation and or prepared upon request for each member of the
Armed Forces and for nonmilitary personnel receiving immunizations, including date, immunization given, dose, and
the initials of the person administering the vaccine. The form contains valid certificates of immunization for interna-
tional travel and quarantine purposes in accordance with WHO international health regulations. CDC Form 731 remains
in the custody of the individual who is responsible for its safekeeping and for keeping it in his or her possession when
traveling internationally. Data are entered by hand, rubber stamp, or by typewriter.
(a) Supply. CDC Form 731 is obtained through normal publication supply channels.
(b) Stamps. Use in accordance with instructions received from the Division of Global Migration and Quarantine; the
appropriate surgeon general; Chief, Bureau of Medicine and Surgery; or CG–11.
1. Army. USAHRC (AHRC–PDR), 1600 Spear Head Division Avenue, Fort Knox, KY 40122.
2. Navy. Bureau of Medicine and Surgery (BUMED), Washington, DC 20372.
3. Air Force. HQ AFPC/DPMDB, Randolph AFB, TX 78148.
7AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
4. Marine Corps. Headquarters, U.S. Marine Corps, Washington, DC 20380.
5 . C o a s t G u a r d . C o m m a n d a n t , C G – 1 1 , U S C G H e a d q u a r t e r s , 2 1 0 0 S e c o n d S t r e e t S W , W a s h i n g t o n , D C
20593–0001.
(c) Written signatures. Written signatures must appear in appropriate spaces on each certificate; signature stamps are
not valid.
c. Lost immunization records. If an individual’s immunization records are lost, assume the individual received
standard immunizations administered at entry into Military Service by the individual’s accession source (for example,
enlisted, Service academy, direct commission) unless there is an objective reason to believe otherwise. Do not repeat
such immunizations. Base decisions for future immunizations on assumed date of last immunization (for example,
individual assumed to have received tetanus-diphtheria toxoid in July 1995 would next be immunized in July 2005).
d. National Vaccine Injury Compensation Program.
(1) The statute 42 USC 300aa-1 to 300aa-34 (The National Childhood Vaccine Injury Act of 1986) and other
regulations set standards for certain immunizations. These requirements apply to U.S. vaccines as indicated by the
CDC after the DHHS Secretary publishes a notice of coverage. Document the patient’s name; identifying number (for
example, sponsor’s SSN); type of vaccine; date of administration; manufacturer; lot number; and the name, address,
and title of person administering the vaccine in a permanent health record or permanent office log or file, in either
paper or electronic format. The electronic immunization tracking systems are the primary method of immunization
documentation. Other records and management reports may be generated from the electronic immunization database, as
described above.
(2) Personnel who administer any vaccine covered under the NVIC program, to either children or adults, will
provide a written copy of the VIS to the vaccinee and allow sufficient opportunity to read the most recent VISs
provided by the DHHS and an opportunity to ask questions about the vaccine. Copies of VISs are available through the
CDC Web site (http://www.cdc.gov/vaccines). The VIS should be supplemented with an oral explanation or video
presentation, or in the appropriate language, when the patient or guardian does not appear to be literate in English.
Provide printed copies to any individual who requests one. Translations of VISs into languages other than English are
available from nongovernmental organizations.
(3) Personnel who administer vaccines are not required to obtain the signature of the military member, patient, or
legal representative acknowledging receipt of a VIS. However, to create a record that the materials were provided,
health care personnel who administer vaccines will annotate each patient’s health record that the VISs were provided at
the time of immunization.
(4) The statute 42 USC 300aa-1 to 300aa-34 (The National Childhood Vaccine Injury Act of 1986), requires that the
following events be reported to VAERS, a public health activity administered by the FDA and CDC:
(a) Any event listed in the NVIC program’s vaccine injury table (at http://www.hrsa.gov/vaccinecompensation/table.
htm) occurring within the time period specified.
(b) Any contraindicating event listed in a vaccine’s package insert (product labeling).
(5) The VAERS accepts all reports by any interested party of real or suspected adverse events occurring after the
administration of any vaccine.
(6) All DOD and USCG health care beneficiaries are eligible to file claims with the NVIC program, according to
the program’s procedures.
2–8. Jet-injection immunization devices
These devices must be used in accordance with FDA-approved manufacturer’s recommendations. Only vaccines with
FDA approval for jet injectors use may be used in these devices.
2–9. Emergency response requirements
a. Written plan. Clinics or activities administering immunizations will develop and maintain a written plan for
emergency response, including standing orders for the management of anaphylaxis and fainting.
b. Training. Whenever vaccines are administered, at least one person present must be trained and current in basic
cardiopulmonary resuscitation, oropharyngeal airway management, and recognition and initial treatment of anaphylaxis
with epinephrine.
c. Anaphylaxis management. For the medical management of an anaphylaxis event whenever vaccines are adminis-
tered, the following must be immediately accessible on scene: stethoscope, blood pressure cuff (sphygmomanometer),
minimum of three adult doses of epinephrine (1:1000), oral airway, bag valve mask or equipment to administer oxygen
by positive pressure, and the equipment and ability to activate an emergency medical system. Other equipment and/or
medications (for example, injectable antihistamines, corticosteroids, vasopressors, glucagon, albuterol, and IV fluids
with administration sets), depending on the clinical setting and local policy, may be included beyond the minimum
requirements listed above.
d. Observation. The ACIP general recommendations suggest that persons be observed for 15 to 20 minutes after
8 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
being immunized. Manufacturer’s guidance must be followed when the manufacturer’s package insert exceeds this
requirement.
2–10. Adverse events
a. Describe in the individual’s health record a detailed account of adverse events after administering immunizing
agents or other medications. Mandatory information consists of identification, lot number, and manufacturer of the
vaccine or other medication; date of administration; name and location of the medical facility; the type and severity of
the event; treatment provided; and any exemption from additional doses. Consultation through MILVAX’s Vaccine
Healthcare Centers network is available 24 hours a day, 7 days a week, for providers who require additional support
for clinical evaluation of possible vaccine adverse events.
b. Health care providers will report adverse events involving vaccines via the VAERS Web site http://www.vaers.
hhs.gov or by faxing or mailing a VAERS–1 form. Obtain VAERS forms and information by calling 1–800–822–7967
or by accessing the VAERS Web site.
c. Health care providers will report adverse events involving chemoprophylaxis agents to MedWatch via the Web
site at http://www.fda.gov/Safety/MedWatch/default.htm or on FDA Form 3500. MedWatch forms and information are
available by calling 1–888–463–6332 or on the MedWatch Web site.
d. Reporting requirements are as follows:
(1) Report adverse events resulting in hospitalization, a life-threatening event (for example, anaphylaxis), time lost
from duty more than one duty shift, or an event related to suspected contamination of a vaccine vial. Reports are also
required for all events listed on the VAERS Table of Reportable Events Following Vaccination (available at http://
vaers.hhs.gov/resources/vaersmaterialspublications).
(2) Further, health care providers are encouraged to report other adverse events considered unexpected in nature or
severity.
(3) Reports of mild expected reactions are not required (for example, low-grade, self-limited fever of less than 24
hours duration, temporary local soreness, redness, or minor swelling at the site of immunization), but such reports may
be submitted if the clinician or patient wishes.
e. Patients may also submit a VAERS or MedWatch report directly. If a patient wishes to submit a VAERS report,
health care personnel will assist the patient in completing the form, regardless of professional judgment about causal
association to immunization.
f. Record pertinent information from the recipient’s health record on the VAERS or MedWatch report. Submit
copies of the report within 7 days of adverse event recognition as follows:
(1) Send the original report form to the VAERS or MedWatch office.
(2) File a copy of the VAERS or MedWatch report in the patient’s individual health record or annotate the relevant
information on the report within the health record.
g. Immediately notify USAMMA or the vaccine manufacturer if contamination or other serious problem with a
vaccine vial or lot is suspected. Suspend usage, but quarantine and retain all such opened or unopened vials or lots
under appropriate storage conditions pending further investigation and disposition instructions.
h. An adverse reaction to a DOD-directed immunization in Service personnel is a line-of-duty condition.
(1) Medical treatment facility (MTF) commanders will provide full access to reserve component (National Guard
a n d R e s e r v e ) m e m b e r s f o r e v a l u a t i o n a n d t r e a t m e n t o f a d v e r s e e v e n t s p o t e n t i a l l y r e l a t e d t o D O D - d i r e c t e d
immunizations.
(2) Reserve component (National Guard and Reserve) unit commanders will inform their members that they may
seek medical care for such adverse events, with the unit providing assistance and information related to pay status and
compensation issues. Any necessary documentation, including line-of-duty determinations, will be completed after the
Reserve component Servicemember is evaluated and, if required, treated. In no case will such evaluation or treatment
be denied or delayed pending line-of-duty determination. If additional health care is required after the initial visit and a
line-of-duty determination has established a Service connection, a notice of eligibility must be completed in accordance
with DODD 1241.01.
(3) DOD will provide an immunization health care capability to deliver medical specialty consultation, case
management, and clinical investigation.
2–11. Program evaluation
MTF facilities and commands storing service treatment records will review immunization and chemoprophylaxis
practices at least annually to ensure compliance with current standards of care and documentation and as a measure of
medical readiness and health promotion. Program evaluation includes internal and external assessments of the standards
for military immunization (see app B). Program evaluation is focused at the clinic level, regardless of Service, to
include both fixed facilities and field units. The Continuous Quality Immunization Improvement Process Tool is one of
several tools available to assist with program evaluation and is described at http://www.vaccines.mil/cqiip. MILVAX
9AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
can assist with guidance and implementation of the Continuous Quality Immunization Improvement Process Tool.
Other tools may be available depending on the Service.
2–12. Blood donation
For timing of immunization with regard to blood donations, clinicians will consider the policies of the Armed Services
Blood Program Office (http://www.militaryblood.DOD.mil) and the specific Service Blood Program Offices. In some
situations, such as accession sites where blood donations are scheduled, regularly coordinate the administration of live
vaccine immunizations after scheduled blood donation activities, when possible.
Chapter 3
Personnel Subject to Immunization
3–1. Military accessions
a. Military accessions. Accessions include Service personnel in enlisted initial entry training, Reserve Officers
Training Corps (ROTC), Officer Candidate School, academy preparatory school, Service academy, Officer Indoctrina-
tion School, other officer accession programs, and officers who are directly commissioned.
(1) When determining the immunization needs of accessions, give credit for immunizations appropriately docu-
m e n t e d e a r l i e r i n l i f e ( f o r e x a m p l e , d a t a f r o m e l e c t r o n i c i m m u n i z a t i o n r e g i s t r i e s m a i n t a i n e d b y S t a t e h e a l t h
departments).
(2) Immunize if the primary series is incomplete, if a booster immunization is needed, or if the Service personnel
has no serologic or documented evidence of immunity. Complete multiple-dose immunization series according to the
recommended schedule as soon as possible.
(3) Before immunizing, conduct serologic testing where available. At a minimum, conduct serologic testing for
antibodies for measles, rubella, hepatitis A, hepatitis B, and varicella. Document medical exemptions for immunity
(MI) in Service ITS. Documented medical exemptions for immunity will be accepted as evidence of immunity in lieu
of vaccination.
(4) Except in an outbreak setting or for individual clinical purposes, immunization records will not be screened after
completion of initial training with regard to measles, mumps, and rubella (MMR), poliovirus, or varicella vaccines.
(5) Document immunizations and immunization exemption codes (medical or administrative) in a DOD-approved
Service ITS.
b. Enlisted accessions. Enlisted accessions may be scheduled for immunizations in two or more clusters, as long as
all appropriate immunizations are administered or seroimmunity is determined. Pregnancy screening or testing for
female accessions must be verified prior to administration of any live virus vaccines.
(1) First cluster. The first cluster of immunizations is administered, if susceptible, before or at the beginning of
collective training (initial entry training, basic military training) to protect against pathogens that represent an imminent
risk of contagious disease in settings of close contact: adenovirus; influenza; meningococcal; MMR; tetanus-diphtheria-
pertussis; and varicella. Pneumococcal vaccine may be administered if warranted epidemiologically. Ensure live virus
vaccines are given on the same day or at least 28 days apart (see ACIP guidelines for exceptions).
(2) Second cluster. The second cluster of immunizations may be administered, if susceptible, in the first or second
half of basic military training, during advanced individual training, or upon arriving at the first duty station to protect
against travel and other military risks. These immunizations include hepatitis A, hepatitis B, influenza (if not
administered in first cluster), and poliovirus. Live virus immunizations follow at least 28 days after earlier live virus
immunizations (see ACIP guidelines for exceptions).
c. Reserve Officers’ Training Corps cadets and midshipmen. ROTC cadets and midshipmen and similar officer
candidates who are ordered or called to active duty or active duty for training will require immunizations. Cadets and
midshipmen may be scheduled for immunizations in two or more clusters:
(1) First cluster. Assess immunization or immunity status and administer immunizations, if susceptible, before or at
the beginning of collective training to protect against pathogens that represent an imminent risk of contagious disease
in settings of close contact. These immunizations include: influenza; meningococcal; MMR; tetanus-diphtheria-pertus-
sis; and varicella. Ensure live virus vaccines are given on the same day or at least 28 days apart (see ACIP guidelines
for exceptions).
(2) Second cluster. The second cluster of immunizations may be administered, if susceptible, in the first or second
half of collective training to protect against travel and other military risks. These immunizations include hepatitis A,
hepatitis B, influenza (if not administered in first cluster), and poliovirus. Live virus immunizations follow at least 28
days after earlier live virus immunizations (see ACIP guidelines for exceptions). ROTC cadets or midshipmen who
travel overseas as part of their training will receive immunizations according to geographic risk assessments.
d. Service academy cadets and midshipmen. Service academy cadets and midshipmen will require immunizations as
follows:
10 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
(1) First cluster. Assess immunization or immunity status and administer immunizations, if susceptible, before or at
the beginning of collective training to protect against pathogens that represent an imminent risk of contagious disease
in settings of close contact. These immunizations include: influenza, meningococcal, MMR, tetanus-diphtheria-pertus-
sis, and varicella. Ensure live virus vaccines are given on the same day or at least 28 days apart (see ACIP guidelines
for exceptions).
(2) Second cluster. The second cluster of immunizations may be administered, if susceptible, in the first or second
half of collective training to protect against travel and other military risks. These immunizations include hepatitis A,
hepatitis B, influenza (if not administered in first cluster), and poliovirus. Live virus immunizations follow at least 28
days after earlier live virus immunizations (see ACIP guidelines for exceptions). Cadets and midshipmen who travel
overseas as part of their training will receive immunizations according to geographic risk assessments.
e. Entry-level officers. Upon accession, screen commissioned and warrant officers for immunization or immunity
status and vaccinate as required.
3–2. Military personnel
a. Active duty personnel. Immunize active duty personnel in accordance with appendix D or as supplemented in
official notices posted at the Military Vaccine Office Web site, http://www.vaccines.mil. During Military Service,
active duty personnel will receive or be up-to-date on adult routine immunizations.
b. Reserve component (National Guard and Reserve). Immunize Reserve component Servicemembers in accordance
with appendix D or as supplemented in Service-specific policies and notices posted at http://www.vaccines.mil.
Reserve component Servicemembers receive the same immunizations as active duty personnel, but must be in a duty
status to receive required immunizations.
c. Aviation personnel. Typically, aviation personnel are grounded for 12 hours (Air Force: access to medical care 4
hours post vaccination unless operational needs dictate otherwise; Navy: refer to “Aeromedical Reference and Waiver
Guide” (ARWG) for vaccine specific information) after immunization, or as specified by their flight surgeon. No
formal grounding documents are required for uncomplicated immunization. Personnel who previously experienced
urticaria, hypersensitivity phenomena, or other unusual phenomena after an immunization are restricted from flying
duty for an appropriate interval (for example, 72 hours) as determined by the flight surgeon. Additional temporary
grounding may be necessary until significant side effects resolve.
d. Occupational risk. Military members at occupational risk for specific disease threats will receive appropriate
vaccines per appendix D or as supplemented in Service-specific policies posted at http://www.vaccines.mil. Immunize
special populations at occupational risk for vaccine-preventable diseases not listed in appendix D per Service, Federal,
State, or local occupational medicine guidance.
e. Geographic travel requirements.
(1) Each Service’s preventive medicine authority maintains current health threat assessments based on disease
prevalence in specific geographical regions using Federal, DOD, USCG, and other relevant sources of information.
These assessments are disseminated to units within their respective jurisdictions. Special Operations may determine
additional area-specific immunization requirements.
(2) Installations and deployed units report disease occurrence through appropriate unit and/or medical lines of
communication.
(3) Combatant commanders, in coordination with the appropriate surgeons general or CG–11, establish specific
immunization requirements based on a disease threat assessment. These requirements may differ from standard Service
immunization policies for personnel entering their area of responsibility to participate in exercises or other operational
missions. Immunize personnel on official deployment or travel orders in accordance with the specific guidance
established by the combatant commander before departure.
(4) For short notice travel or deployments requiring vaccines given in a multi-dose series, administer the first dose
of the basic series. Administer as many of the subsequent doses as time permits. Completion before departure is the
goal. If the series cannot be completed before departure, complete it upon arrival. Inform the patient that in order to
obtain optimal immunity, the series must be completed by receiving all the required doses at the recommended
intervals.
(5) For quarantine, entry, and reentry requirements, follow the provisions of the CDC, Division of Global Migration
and Quarantine regulations concerning entry or reentry of military and nonmilitary personnel into the United States or
its commonwealths, territories, and possessions.
f. Other uniformed Service personnel. Members of other uniformed Services are authorized immunizations according
to their occupation, official duties, travel plans, health status, or other relevant factors.
3–3. Certain civilian employees
a. Federal civilian employees.
(1) General. Federal civilian employees will receive country-specific immunizations without charge at military
activities upon presentation of official orders or authorization. Area preventive medicine authorities are consulted for
recommendations applicable to specific areas. People declining immunizations required for entry into foreign countries
11AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
are referred to the appropriate authority for counseling. Document counseling in the health record and note that
omission of certain immunizations may have consequences under host country policies, which could include compul-
sory immunization, detention, quarantine, or denial of entry.
(2) Civilian employees at occupational risk for vaccine-preventable disease. Federal civilian employees who are at
risk of exposure to an infectious disease associated with their occupation may receive appropriate immunizations,
without charge, at military activities. Administer immunizations upon recommendation of the responsible occupational
medicine authority.
(3) Civilian health care employees. Susceptible or occupationally exposed health care employees (including volun-
teers) who are at risk of exposure to an infectious disease (for example, influenza) associated with their occupation
may receive appropriate immunizations, without charge, at military activities. This policy applies to all health care
settings, regardless of age or sex of the health care employee. Employees, including volunteers, who have contact with
or potential exposure to human blood or blood products (whether from patient care, laboratory, or other health care
settings) are provided hepatitis B virus vaccine in accordance with the local bloodborne pathogen exposure-control
plan. Refer to the Occupational Safety and Health Administration standards (29 CFR 1910.1030) for additional
information. Immunizations or immune status may be a condition of employment.
(4) Employees with potential occupational exposure to wastewater or sewage. Employees at occupational risk of
exposure to wastewater or sewage will receive tetanus-diphtheria toxoids (preferably with pertussis vaccine) per ACIP
recommendations. Other vaccines are not routinely required based solely on occupational exposure for wastewater
treatment system workers, including sewage generated by medical facilities.
(5) Individuals immunized per categories above. Individuals immunized per the civilian personnel categories above
are authorized treatment and necessary medical care related to adverse events after immunization, consistent with
applicable occupational health program requirements.
b. Civilian Expeditionary Workforce. Civilian employees and others in the Civilian Expeditionary Workforce may
receive, without charge, appropriate immunizations at military activities. In accordance with DODD 1404.10, compo-
nents should ensure emergency-essential and non-combat essential employees are aware of potential deployment
immunizations as a condition of employment. Components should also ensure the employee completes and signs a
record of notification with a signed DD Form 2365 (DOD Civilian Employee Overseas Emergency-Essential Position
Agreement). Applicable vacancy announcements and position descriptions will note obligations to receive immuniza-
tions. Emergency-essential and non-combat essential employees have the same access as military personnel to treat-
ment and necessary medical care related to adverse events after immunization, consistent with applicable occupational
health program requirements.
c. Bargaining units. For Federal employees in a bargaining unit, local management must meet applicable labor
relations obligations before implementing any changes to the bargaining unit employees’ conditions of employment.
Civilian personnel advisory centers provide guidance on these matters.
d. Biological warfare defense. Immunization of civilian employees and contracted workers for biological warfare
defense are addressed in DODI 6205.4.
e. Emergency situations. In emergency situations, the provisions of DODD 6200.03 apply.
3–4. Contracted workers
a. Provide immunizations to contracted workers according to the terms of the contract and as stated in the contract
agreement. If the contract does not provide for provision of immunizations by the government, contractors are
responsible for providing appropriate immunizations to their employees For vaccines with limited distribution (for
example, anthrax, smallpox), DOD or USCG may provide the immunizations, regardless of the terms of the contract.
The contractor is responsible for work-related illnesses, injuries, or disabilities under worker-compensation programs,
supplemented by existing Secretarial designee authority.
b. Contracted health care workers are eligible for immunizations required or offered to health care employees and
are provided as stated in the contract agreement. Contracts will include specifications describing immunizations
required of contracted health care workers.
c. Family members of contracted workers in foreign-duty settings under military sponsorship will receive country-
specific immunizations without charge at military activities upon presentation of official orders or authorization. People
declining immunizations required for entry into foreign countries are referred to the appropriate authority for counsel-
ing. Document counseling in the health record and note that omission of certain immunizations may subject them to
adverse action according to host country policies, which could include compulsory immunization, detention, quarantine,
or denial of entry.
3–5. Department of Defense, U.S. Coast Guard schools, childcare centers and youth programs
a. As a condition of employment, schoolteachers, childcare center workers, youth program workers, and volunteers
are administered appropriate vaccines against communicable diseases in accordance with ACIP adult immunization
schedule recommendations, unless already immune, based on seroimmunity, physician diagnosed illness, or docu-
mented proof of immunization.
12 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
b. Children attending DOD and USCG-sponsored primary and secondary schools, childcare centers, or similar
facilities are required to be up to date on all age appropriate ACIP-recommended vaccines for children unless there is
documentation of previous immunization, religious exemption, or medical contraindication. For foreign-national chil-
dren outside the United States, observe host country recommendations or requirements.
3–6. Other populations
a. Department of Defense and U.S. Coast Guard beneficiaries.
(1) Family members of military personnel. Family members receive immunizations according to current ACIP
recommendations. In addition, Family members may be subject to Service-specific requirements and recommendations
for immunizations applicable to the country in which they will reside while accompanying military members under
military sponsorship.
(2) Family members or sponsored individuals of other Federal civilian employees in foreign-duty settings under
military sponsorship. These Family members will receive country-specific immunizations without charge at military
activities upon presentation of official orders or authorization. People declining immunizations required for entry into
foreign countries are referred to the appropriate authority for counseling. Document counseling in the health record and
note that omission of certain immunizations may have consequences under host country policies, which could include
compulsory immunization, detention, quarantine, or denial of entry.
b. Foreign nationals. Foreign nationals who come to the United States, its territories, commonwealths, or posses-
sions under Armed Forces sponsorship receive immunizations required for entry into the United States and by local
jurisdictions. When returning to their country of origin, foreign nationals receive immunizations required by interna-
tional health regulations or their country of origin. These immunizations are administered without charge at military
activities upon presentation of official orders or authorization.
c. Detainees. The installation or activity commander, upon the recommendation of the appropriate medical authority,
will provide immunizations against diseases that may be a significant cause of death or illness among detainees. Such
immunizations are voluntary and are administered without charge to the detainee. Annotate all immunizations and
chemoprophylactic medications in the detainee’s health record. Before immunization, inform detainees in their own
language about the relative benefits and risks of the specific immunizations offered. Factors to consider in deciding
which immunizations to offer detainees include their likely preexisting immunity, the anticipated length of detention,
seasonal threat of infection, and other risk factors related to personal health status and living conditions. (Refer to
DODI 2310.08E for additional guidance.)
d. Overseas commander authority. The overseas commander, commanding officer, or officer-in-charge, upon the
recommendation of the appropriate medical authority, will provide immunizations against communicable diseases
judged to be a potential hazard to the health of the command; such vaccines are administered without charge.
e. Other than U.S. Forces. Immunization of other than U.S. Forces for biological warfare defense are addressed in
DODI 6205.4.
f. Emergency situations. In emergency situations, the provisions of DODD 6200.03 apply.
Chapter 4
Specific Immunization Requirements for Department of Defense and U.S. Coast Guard
Personnel
(Also see appendix D for a chart on the required immunizations for military personnel.)
4–1. Civilian applicability
Certain civilian employees may be required to receive immunizations as a condition of their employment or participa-
tion in a particular assignment. In such cases, failure to voluntarily receive the immunizations may result in a personnel
action being taken (see chap 3), but in no case will immunizations be involuntarily administered.
4–2. Adenovirus types 4 and 7
a. Military indication. To prevent adenovirus infection, an acute febrile respiratory disease caused by adenovirus
serotypes 4 and 7. Direct contact and fecal oral transmission of the virus may result in a respiratory disease infection or
outbreak of disease among an unvaccinated recruit population.
b. Basic trainees. Administer adenovirus vaccine to military enlisted basic trainees before or at the beginning of
collective training at the same time the first live virus vaccines are administered. Routine administration in other
populations is not generally recommended except when directed by preventive medicine guidance, based on disease
incidence and severity.
4–3. Anthrax
a. Military indication. To prevent anthrax, an acute infectious disease caused by the spore forming bacterium
13AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Bacillus anthracis. Direct exposure to anthrax spores may result in cutaneous, gastrointestinal, or inhalational infection.
Bacillus anthracis has been identified as a potential biological warfare agent.
b. Military and civilian personnel. Administer anthrax vaccine to military personnel and applicable civilians accord-
ing to DOD or USCG policy for the Anthrax Vaccine Immunization Program and Service-specific implementation
plans. Immunize personnel based on geographical areas at higher risk for release of anthrax as a weapon or in
occupational roles as designated by the Services, Chairman of the Joint Chiefs, or the Office of the Secretary of
Defense.
c. Occupational risk. Administer anthrax vaccine to at-risk veterinary and laboratory workers and others at occupa-
tional risk of exposure.
4–4. Haemophilus influenzae serotype b, commonly called Hib
a. Military indication. To prevent invasive Haemophilus influenza disease and infection of many organ systems
caused by the bacterium Haemophilus influenzae serotype b (Hib). The disease is transmitted via respiratory droplets.
The most common types of invasive Hib disease are: meningitis, epiglottitis, pneumonia, arthritis, and cellulitis.
b. Military and civilian personnel. Administer Hib vaccine to those who are immunocompromised, have sickle cell
disease, or do not have a spleen or a functioning spleen.
4–5. Hepatitis A
a. Military indication. To prevent hepatitis A, an acute infection of the liver that is acquired by consuming food or
water contaminated with hepatitis A virus, particularly during deployment or travel to areas with poor food, water, and
sewage sanitation. It can range in severity from a mild illness lasting a few weeks to a severe illness lasting several
months. Hepatitis A infections occur worldwide.
b. Basic trainees and other accessions. Unless seroimmune, administer hepatitis A vaccine to trainees and acces-
sions during initial entry training.
c. Military and civilian personnel. Unless seroimmune, or evidence of appropriate complete vaccination, administer
hepatitis A vaccine to all military personnel, and civilian personnel when indicated.
d. Occupational risk. Hepatitis A vaccine is indicated per ACIP guidelines and locally designated food handlers.
4–6. Hepatitis B
a. Military indication. To prevent hepatitis B, an acute or potentially chronic infection of the liver that is acquired
through percutaneous, sexual, and other mucosal exposure to blood and body fluids from people infected with hepatitis
B virus. Chronic infections may result in cirrhosis or cancer of the liver. Hepatitis B infections occur worldwide, and
some infected people maintain a chronic carrier state.
b. Basic trainees and other accessions. Unless seroimmune, administer hepatitis B vaccine to basic trainees and
accessions during initial entry training.
c. Military and civilian personnel. Unless seroimmune, or evidence of appropriate complete vaccination, administer
hepatitis B vaccine to all military personnel, and civilian personnel, when indicated.
d. Occupational risk. Administer hepatitis B vaccine to susceptible personnel who are at risk of potential exposure
to bloodborne pathogens per the Occupational Safety and Health Administration standards (29 CFR 1910.1030). For
military purposes, this includes occupational specialties involving health care workers, emergency medical technicians,
mortuary affairs personnel, search and rescue specialists, correctional facility staff, and designated special operations
forces.
e. Serologic testing. Conduct serologic testing of health care workers who have direct contact with patients and
those who have potential occupational risk for exposure to bloodborne pathogens 1 to 2 months after completion of the
hepatitis B vaccine series to determine serologic response according to CDC and ACIP recommendations.
4–7. Influenza
a. Military indication. To prevent influenza, an acute febrile respiratory viral infection that can cause epidemics
within military populations, especially under conditions of crowding, such as initial entry training, aboard ships,
extended air transport, or deployment settings. Influenza has the potential for widespread transmission through person-
to-person contact and fomites.
b. Military personnel. Administer influenza vaccine(s) annually or as indicated to all active duty, Reserve, and
National Guard personnel.
c. Occupational risk. Administer influenza vaccine(s) annually or as indicated to personnel who work or volunteer
in DOD MTFs.
4–8. Japanese encephalitis
a. Military indication. To prevent Japanese encephalitis, a mosquito-borne viral disease, during deployments and
travel to endemic areas in Eastern Asia and certain western Pacific Islands. Japanese encephalitis virus (JEV) can cause
14 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
an acute infection of the brain, spinal cord, and meninges with high rates of complications, chronic disability, and
death.
b. Military and civilian personnel. Administer the JEV vaccine to military personnel and civilian personnel who
have a substantial risk of exposure to the virus based on their geographic location.
c. Temporary flying restrictions. Impose temporary flying restrictions post-JEV immunization for aircrew personnel
per Service-specific policy.
4–9. Measles, mumps, and rubella (MMR)
a. Military indication. To prevent MMR, primarily by boosting immunity acquired from childhood immunization.
These three acute viral infections are spread by the respiratory route or person-to-person contact. In military trainee
populations, each can cause disease outbreaks. Rubella usually causes a mild infection, but infection during the first
trimester of pregnancy puts the fetus at high risk of congenital rubella syndrome and birth defects. Young adults may
experience more severe complications from mumps infection. All three diseases occur worldwide, primarily among
children.
b. Basic trainees and other accessions. Unless seroimmune to both measles and rubella, administer MMR vaccine to
susceptible basic trainees and accessions within the first 2 weeks of training.
c. Military and civilian personnel. Presume immunity through infection for persons born in 1957 or earlier. Ensure
personnel born after 1957 have received two lifetime doses of MMR vaccine or have positive serologic test results.
Immunity against mumps is not necessary as a military requirement, but may be appropriate in exceptional clinical
circumstances such as outbreaks.
d. Occupational risk. Ensure health care workers have received two documented doses of MMR vaccine or have
positive serologic test results.
4–10. Meningococcal
a. Military indication. To prevent meningococcal disease or meningitis and other systemic infections caused by the
bacteria Neisseria meningitidis serogroups A, C, W–135, and Y. No vaccine against serogroup B meningococcus,
another common pathogen, is currently licensed in the United States. Basic trainees and other military populations
living in crowded conditions are at an increased risk for meningococcal infection. Historically, outbreaks have occurred
in training populations. Meningococcal vaccine may be indicated for deployment and travel to areas with highly
endemic meningococcal disease.
b. Basic trainees and other accessions. Administer meningococcal vaccine to basic trainees, cadets, and midshipmen
at Service academies within the first 2 weeks of training, if no evidence of vaccination within the last 5 years.
c. Military and civilian personnel. Administer meningococcal vaccine to personnel traveling to countries in which N.
meningitidis is hyperendemic or epidemic and other countries as required by DOD and USCG policy or recommended
by the CDC.
d. Alert personnel. Administer meningococcal vaccine to personnel who are designated to deploy within 10 days of
notification.
e. Other personnel. Administer one dose of meningococcal vaccine to persons who do not have spleens or functional
spleens.
4–11. Pertussis
Tetanus, diphtheria, and pertussis guidance is in paragraph 4–16.
4–12. Pneumococcal
a. Military indication. To prevent pneumococcal disease due to Streptococcus pneumoniae in personnel who fall
into a high-risk category due to age or underlying health conditions (for example, persons who smoke, have asthma, or
have no spleen) or who are in high-risk situations, such as certain training populations. Streptococcus pneumoniae may
result in pneumonia, bacteremia, and meningitis.
b. Basic trainees and other accessions. Routine administration of vaccine is not generally practiced, but may be
directed by preventive medicine guidance, based on disease incidence and severity.
c. Military personnel. Administer pneumococcal vaccine to military personnel who are in a high-risk category per
ACIP recommendations. Administer a second dose to persons without spleens or severely immunocompromised five
years after the initial dose.
4–13. Poliomyelitis
a. Military indication. To prevent poliomyelitis, a viral infection that affects the central nervous system resulting in
paralytic symptoms, primarily by boosting immunity acquired from childhood immunization. Poliomyelitis is acquired
by person-to-person transmission through the fecal-oral route. Military and civilian personnel deploying or traveling to
areas with poor sanitation are at increased risk, although international immunization efforts have decreased poliomyeli-
tis incidence worldwide. Only inactivated poliovirus vaccine (IPV) is available in the US.
15AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
b. Basic trainees and other accessions. Administer a single booster dose of IPV to basic trainees and accessions.
Personnel who have not received the primary series must complete the series using IPV. Unless there is reason to
suspect otherwise (for example, childhood spent in a developing country, childhood immunizations not administered),
receipt of the primary series of IPV may be assumed.
c. Military personnel. Because of the high level of childhood immunization against this disease, do not screen
immunization records with regard to poliovirus immunity after completion of initial entry training except in an
outbreak setting or for individual clinical purposes.
4–14. Rabies
a. Military indication. To prevent rabies, a life threatening viral disease caused by exposure to the saliva of animals
or humans infected with the rabies virus, which includes bites.
(1) Pre-exposure prophylactic immunization. A pre-exposure immunization series may be indicated for people with
potential occupational risk of exposure to rabid animals, or for forces assigned to locations where access to definitive
care likely exceeds 24 hours. Pre-exposure prophylaxis should not be considered sufficient for the prevention of rabies;
however, it reduces the need for human rabies immune globulin-better known as HRIG-and reduces the number of
shots required for post-exposure prophylaxis.
(2) Post-exposure prophylaxis. Consult with a preventive medicine physician and veterinarian for guidance and to
report the animal exposure. Post-exposure treatment includes immediate wound care, and may include the post-
exposure vaccine series, and human rabies immune globulin in an unvaccinated patient. Post-exposure prophylaxis is
safe and effective.
b. Military personnel. Administer pre-exposure rabies vaccine series to special operations personnel, including
designated special operations enablers and the occupational risk groups listed below, in accordance with Service policy.
c. Occupational risk. Administer pre-exposure rabies vaccine series to veterinary workers, animal handlers, certain
laboratory workers, and personnel who have animal control duties and personnel assigned long-term to regions with
endemic rabies. Give booster doses every 2 years or when antibody concentrations indicate.
4–15. Smallpox
a. Military indication. To prevent smallpox disease due to the deliberate release or spread of the smallpox virus. In
1980, the WHO declared the global eradication of naturally occurring smallpox. Nonetheless, stocks of variola virus,
the causative agent of smallpox, could be used as a biological warfare agent.
b. Military and civilian personnel. Vaccinate designated military and civilian personnel according to DOD and other
designed personnel in accordance with USCG policy and Service-specific implementation plans. These include military
personnel and applicable civilians who are smallpox epidemic response team members, assigned to medical teams at
hospitals and clinics, or assigned to designated forces that constitute mission-critical capabilities. Immunize personnel
based on geographical areas at higher risk for release of smallpox as a weapon or in occupational roles as designated
by the Services, Chairman of the Joint Chiefs, or the Office of the Secretary of Defense.
c. Training and education. Before administering smallpox vaccine to military or civilian personnel who are eligible
to receive smallpox vaccine, provide education on the criteria for exemption from immunization, expected response at
the vaccination site, vaccination-site care, risks of spreading vaccinia to close contacts, adverse events following
immunizations (AEFI) such as myopericarditis, and other relevant topics per Service implementation plans.
d. Screening. Use the DOD-specific screening form posted at http://www.vaccines.mil to identify persons with
personal or household contraindications to smallpox vaccination (for example heart conditions, immunosuppressed
conditions, pregnancy, skin conditions such as eczema and atopic dermatitis). Screening will include assessing
pregnancy status and recency of testing for human immunodeficiency virus infection. In the event of a smallpox
outbreak, “permanent” exemptions may be rescinded according to individual risk of exposure to variola virus.
e. Vaccination. Internal MTF and command clinical quality management programs will have mechanisms to confirm
that vaccinators demonstrate proper vaccination technique.
f. Post-vaccination site care. Take appropriate care to prevent the spread of vaccinia virus from a vaccinee’s
vaccination site. MTFs will monitor the vaccination sites of vaccinated health care workers (for example, operating
site-care stations), promote effective bandaging, and encourage scrupulous hand washing.
g. Post-vaccination evaluation (“take” check). Assessment and documentation of response (a “take”) to vaccination
is required for health care workers and members of smallpox response teams who would travel into a smallpox
outbreak area. Evaluate and record the vaccination response of individuals receiving smallpox vaccine in a DOD and
USCG-approved electronic ITS.
4–16. Tetanus, diphtheria, and pertussis
a. Military indication. To prevent tetanus, diphtheria, and pertussis, primarily by boosting immunity acquired from
childhood immunization.
(1) Tetanus is an acute disease of the nervous system caused by the serotoxin produced by Clostridium tetani. The
C. tetani spores enter the body through breaks in the skin, and the bacterium then grows at the wound site. A tetanus
16 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
infection results in generalized rigidity and convulsive spasms of the skeletal muscles. The C. tetani spores occur in the
environment worldwide.
(2) Diphtheria is an acute disease caused by a cytotoxin of the bacteria Corynebacterium diphtheriae. C. diphtheriae
is transmitted person-to-person via respiratory droplets and direct contact. Diphtheria can lead to airway obstruction,
and more severe complications may result from toxin absorption into organs and tissues. Diphtheria occurs worldwide.
(3) Pertussis is a highly communicable acute respiratory illness caused by the bacteria Bordetella pertussis. Pertussis
is spread via direct contact with respiratory secretions. Pertussis occurs worldwide.
b. Basic trainees and other accessions. For those individuals lacking a reliable history of prior immunization,
administer one dose of Tetanus-diphtheria and acellular pertussis (Tdap) vaccine according to ACIP guidelines. Unless
there is reason to suspect otherwise (for example, childhood spent in a developing country, childhood immunizations
not administered), receipt of the basic immunizing series may be assumed.
c. Military and civilian personnel. Administer booster doses of Tetanus-diphtheria (Td) to all personnel every 10
years following the completion of the primary three-dose series. A one-time dose of Tdap in place of a Td booster
during adulthood is required, regardless of interval.
d. All personnel. Following ACIP wound-management guidelines for the treatment of contaminated wounds. Tdap is
preferred to Td for adults vaccinated 5 years earlier who require a tetanus toxoid-containing vaccine as part of wound
management and who have not previously received Tdap. For adults previously vaccinated with Tdap, Td should be
used if a tetanus toxoid-containing vaccine is indicated for wound care.
4–17. Typhoid fever
a. Military indication. To prevent typhoid fever, a systemic bacterial disease acquired by consuming food or water
contaminated with Salmonella typhi, particularly during deployment or travel to typhoid-endemic areas and other areas
with poor sanitation.
b. Military and civilian personnel. Administer typhoid vaccine before overseas deployment to typhoid-endemic
areas.
c. Alert personnel. Administer typhoid vaccine to alert personnel, per Service policy, who are prepared for deploy-
ment to typhoid-endemic areas or who have potential risks of exposure to contaminated local food and drink.
Administer booster doses per immunization schedule. For Air Force, only units specifically identified by the MAJCOM
surgeon require initial and subsequent immunization against typhoid fever.
4–18. Varicella
a. Military indication. To prevent varicella (chickenpox), a generally mild and self-limiting viral infection caused by
the varicella zoster virus. Although varicella is a common childhood disease, adults may experience more severe illness
and have higher complication and case-fatality rates. Adolescents and adults are at higher risk for severe disease
complications such as secondary skin infections, neurologic disease, and multi-organ involvement. Varicella zoster
virus is transmitted by respiratory secretions, direct contact, and aerosolization of the virus from skin lesions. Military
members at higher risk for infection include basic trainees, cadets/midshipmen at Service academies, officer trainees,
and special operations personnel, and others living in military environments conducive to person-to-person spread of
respiratory diseases (for example, barracks, ships).
b. Basic trainees and other accessions. Administer varicella vaccine to susceptible trainees and other accessions
within the first 2 weeks of initial entry training. Serologic screening of trainees is the preferred means of determining
those susceptible to varicella infection and in need of immunization. Identify those people who do not have a personal
history of varicella disease, documentation of two prior varicella immunizations, or documentation of immunity based
on serologic testing as susceptible. Document positive results of serologic testing in a DOD-approved electronic ITS.
Adults and adolescents require two doses of varicella vaccine given 4 to 8 weeks apart.
c. Health care workers. Administer varicella vaccine to susceptible health care workers. Determine susceptibility as
noted above for trainees, birth before 1980 should not be considered evidence of immunity for health care workers.
Routine post-immunization testing for antibodies to varicella is not recommended.
d. Other susceptible adults. Offer varicella vaccine to other susceptible persons, especially nonpregnant women of
childbearing age and men living in households with young children.
4–19. Yellow fever
a. Military indication. To prevent yellow fever disease, a viral infection that may result in severe systemic disease
and organ failure. Yellow fever infection is transmitted via the bite of an infected mosquito. Documented vaccination
status must be verified to meet international health requirements during deployment or travel to yellow-fever-endemic
areas. Areas of greatest risk are sub-Saharan Africa and tropical South America.
b. Military personnel. Administer yellow fever vaccine to all Marine Corps accessions and military personnel
traveling to or transiting through yellow-fever-endemic areas.
c. Alert personnel. Administer yellow fever vaccine to alert personnel prepared for deployment to yellow-fever-
endemic areas. Administer booster doses per immunization schedule. For Air Force, only units specifically identified
17AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
by the MAJCOM surgeon require initial and subsequent immunization against yellow fever. For Navy, administer to
those assigned to units subject to deployment within 10 days of notification into land areas where yellow fever is
endemic.
d. Civilian and other personnel. Administer yellow fever vaccine to personnel traveling to, or transiting through,
endemic areas.
Chapter 5
Chemoprophylaxis
5–1. General
a. Chemoprophylaxis. This section does not relate to the treatment of diseases but provides a brief review of military
relevant diseases and associated chemoprophylaxis guidelines. Chemoprophylaxis is defined here as the administration
of medication before, during, or after possible exposure to an infectious agent, to prevent either infection or disease.
Most agents used for chemoprophylaxis are not FDA-approved for this indication and thus may not be administered to
units under a force health protection strategy or policy; rather, these agents must be prescribed to individuals and
documented accordingly by an appropriate health care provider. Follow instructions from the relevant combatant
command surgeon who will consult with the appropriate preventive medicine authority for the use of chemoprophylac-
tic agents. Command medical officers will review indications for use and potential adverse effects of specific
chemoprophylactic medications before use. These recommendations for drugs or agents are current as of the date of
this publication. Consult current information and guidance for appropriate drugs and dosing regimens (for example the
CDC, the ACIP, the National Center for Medical Intelligence (NCMI), and the American Public Health Association’s
“Control of Communicable Diseases Manual”). The following classes of chemoprophylaxis are not addressed in this
publication:
(1) Chemical warfare-related chemoprophylaxis. Consult the current version of “Medical Management of Chemical
Casualties,” published by the U.S. Army Medical Research Institute of Chemical Defense.
(2) Medical therapy for tuberculosis infection. Consult publications from CDC, the American Thoracic Society, the
Advisory Council for the Elimination of Tuberculosis, and similar authorities.
(3) Radiation-related chemoprophylaxis (for example, potassium iodide, granisetron, or Prussian blue).
(4) Other forms of prevention involving nonbiological medications (for example, calcium, aspirin, or vitamins).
(5) Immunotherapy.
b. Packaging. Dispense chemoprophylaxis agents to individuals in child-resistant containers, consistent with 15 USC
1471–1476 (The Poison Prevention Packaging Act), or unit-of-use packaging. Use appropriate packaging to keep the
medication clean and dry.
c. Labeling. Dispense chemoprophylaxis agents to individuals in packages that contain the name of the product,
directions for proper use, and the name of the person to whom the medication was dispensed.
5–2. Anthrax
a. Military indication. The use of antibiotics and immunoglobulin following a possible exposure to anthrax is
locally-directed and is prescribed by preventive medicine based on risk. The use of antibiotics and immunoglobulin
have been shown to increase survival when used after exposure to anthrax and before onset of symptoms (post-
exposure prophylaxis or empiric treatment).
b. Chemoprophylaxis. Recommended drugs include ciprofloxacin and doxycylcine. Refer to Service-specific poli-
cies. Anthrax immunoglobulin is available through the CDC’s Emergency Operation Center.
5–3. Group A streptococcus
a. Military indication. Outbreaks of group A streptococci can spread rapidly in groups in settings of close contact,
such basic training and contingency operations.
b. Chemoprophylaxis. The primary drug used for prophylaxis is penicillin, specifically the long-acting injectable
form, penicillin G benzathine. Oral penicillin VK and azithromycin have also been used effectively. Administer
penicillin prophylactically, when required, to terminate disease transmission. Routine administration of penicillin for
prophylaxis of basic trainees against group A streptococcal infection has been shown to be effective at some
installations with historically high incidence of disease. This practice should be directed by local preventive medicine
authority.
5–4. Influenza
a. Military indication. Influenza can be a significant cause of morbidity in a susceptible population and can degrade
mission capability.
b. Chemoprophylaxis. Consider prophylactic use of antiviral therapy if available vaccine does not antigenically
18 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
match circulating strains or if an outbreak occurs early in the season before widespread immunization. For additional
guidance, refer to CDC.
5–5. Leptospirosis
a. Military indication. Leptospirosis can cause morbidity in personnel exposed to contaminated water sources.
b. Chemoprophylaxis. Doxycycline is effective in preventing leptospirosis in exposed military personnel during
periods of high risk of exposure. Consult an infectious diseases or preventive medicine authority for proper use and
dosing.
5–6. Malaria
a. Military indication. Malaria has caused morbidity and mortality in military populations for centuries. It continues
to be one of the most important disease threats to military and civilian personnel deployed to areas where the disease is
endemic.
b. Chemoprophylaxis. The Services or the combatant command surgeon determine specific chemoprophylactic
regimens, typically with guidance from the NCMI, for the area of operations based on degree and length of exposure
and the prevalence of drug resistant strains of plasmodia in the area(s) of travel. Prescribe anti-malarials per package
insert. Health care providers will screen individuals for contraindications to specific malaria chemoprophylaxis (for
example G6PD deficiency and primaquine) and determine the appropriate malaria chemoprophylaxis. Health care
providers must document malaria chemoprophylaxis prescriptions in the health record when anti-malarial medications
are prescribed. Include the member’s electronic medication profile (for example, Composite Health Care System II),
whenever possible.
5–7. Meningococcal disease
a. Military indication. Meningococcal disease can result in morbidity and potential mortality in populations experi-
encing crowded conditions. Chemoprophylaxis has been shown to prevent disease when administered post-exposure to
susceptible people.
b. Chemoprophylaxis. There are several drugs available for prophylaxis of close contacts of meningococcal disease
cases. Consult an infectious diseases or preventive medicine authority for determination of individuals to offer
prophylaxis and for assistance with drug selection and dosing.
5–8. Plague
a. Military indication. Plague has been identified as a potential biological warfare agent, especially if aerosolized to
c a u s e p n e u m o n i c p l a g u e . T h e r e i s n o l i c e n s e d v a c c i n e t h a t i s e f f e c t i v e a g a i n s t p n e u m o n i c p l a g u e . P r o v i d e
chemoprophylaxis to persons potentially exposed to cases of pneumonic plague.
b. Chemoprophylaxis. Consult an infectious diseases or preventive medicine authority for determination of individu-
als to offer prophylaxis and for assistance with drug selection and dosing.
5–9. Scrub typhus
a. Military indication. Spread by the bite of infective larval mites. Mite bites may be a source of morbidity in
populations encountering field conditions.
b. Chemoprophylaxis. Doxycycline has been shown to be effective in preventing scrub typhus in exposed personnel.
Consult an infectious diseases or preventive medicine authority for proper use and dosing.
5–10. Smallpox
a. Military indication. Various forms of vaccinial infections may develop following receipt of the smallpox vaccine.
Chemoprophylaxis may be indicated to prevent morbidity in immunized Servicemembers or their contacts.
b. Chemoprophylaxis. VIG and vaccinia-specific antivirals are available through the DOD. Contact MILVAX to
request and coordinate administration of these chemoprophylactic agents.
5–11. Traveler’s diarrhea
a. Military indication. Diarrhea can cause morbidity in personnel exposed to contaminated food and water sources.
b. Chemoprophylaxis. Chemoprophylaxis for traveler’s diarrhea is only recommended on rare occasions where
diarrhea would compromise a mission. Prophylactic antibiotics may be considered for short-term travelers who are
high-risk hosts (such as those who are immunosuppressed) or those taking critical trips during which even a short bout
of diarrhea could significantly impact the purpose of the trip. Instead of prophylaxis travelers, should be prescribed
appropriate medications and provided instructions for self-treatment of diarrhea. Consult an infectious diseases or
preventive medicine authority for assistance.
19AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Chapter 6
Biological Warfare Defense
6–1. Responsibilities
a. The combatant commanders, annually and as required, provide the Chairman of the Joint Chiefs of Staff with
their assessment of the biological warfare threats to their theaters.
b. The President of the Defense Health Board, in consultation with the Secretaries of the Military Departments,
annually and as required, identifies to the Assistant Secretary of Defense (Health Affairs) (ASD (HA)) vaccines
available to protect against validated biological warfare threat agents and recommends appropriate immunization
protocols and/or chemoprophylaxis.
6–2. Procedures
The DOD Immunization Program for Biological Warfare Defense is conducted as follows:
a. The combatant commanders, annually and as required, provide the Chairman of the Joint Chiefs of Staff with
their assessment of the biological warfare threats to their theater.
b. The Chairman of the Joint Chiefs of Staff, in consultation with the combatant commanders; the chiefs of the
Military Services; and the Director, Defense Intelligence Agency, annually validates and prioritizes the biological
warfare threats to DOD personnel and forwards the threat list to the DOD Executive Agent through the ASD (HA).
c. Within 30 days of receiving the validated and prioritized biological warfare threat list from the Chairman of the
Joint Chiefs of Staff, the DOD Executive Agent, in consultation with the Secretaries of the military departments and
the President of the Defense Health Board, provides recommendations to the ASD (HA) on vaccines and immunization
protocols necessary to enhance protection against validated biological warfare threat agents.
d. Within 30 days of receiving the coordinated recommendations of the DOD Executive Agent, the ASD (HA)
directs the Secretaries of the military departments to begin immunization of the specified DOD and USCG personnel
against specific biological warfare threat agents. The ASD (HA) will coordinate with and obtain approval from the
Secretary or Deputy Secretary of Defense before issuing the appropriate direction.
e. The Secretaries of the military departments will program and budget for required vaccinations, including the costs
of the biological warfare defense vaccines.
Chapter 7
Vaccines and Other Products in Investigational New Drug Status
7–1. Purpose
For infectious disease threats for which the only available vaccine or chemoprophylaxis product is in an IND status, the
IND product must be administered in full accordance with FDA regulations at 21 CFR Parts 50 and 312, as well as 10
USC 1107, Executive Order 13139, and DODD 6200.2. DOD may use products that have not been approved or
licensed for commercial marketing as force health protection measures in combat settings, other military operations,
peacekeeping, or humanitarian missions. DOD will provide comparable access to IND products to military personnel,
civilian personnel, contracted workers, and beneficiaries based on the health risk to the people involved.
7–2. General guidance on investigational new drug products
Commanders, through the appropriate chain, must request approval from the Secretary of Defense to use INDs for
force health protection. If the member’s use of an IND product is voluntary, the product must be administered with
documented informed consent in accordance with a protocol approved by the FDA for IND product use. A vaccine,
antibiotic, or other product in an IND status may be mandatory for military members, if the President of the United
States has approved a waiver of the requirement for informed consent. Under 10 USC 1107, only the President has the
authority to grant a waiver of the requirement that a military member provide prior consent to receive an IND or a drug
unapproved for its applied use in connection with the member’s participation in a particular military operation. The
President must determine, in writing, that obtaining consent (1) is not feasible, (2) is contrary to the best interests of
the member, or (3) is not in the interests of national security. The requirement for informed consent may not be waived
for civilian personnel, contracted workers, and beneficiaries.
7–3. Health recordkeeping requirements for investigational new drug products
All IND vaccines or chemoprophylaxis products that are administered, whether with the member’s informed consent or
with an approved waiver of informed consent, must be recorded in the individual’s permanent health record or DOD
and USCG-approved electronic ITS. For vaccines, the documentation is the same as that required for other vaccines
with an annotation “IND” with the vaccine name. This recordkeeping requirement is in addition to any recordkeeping
20 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
requirements of the FDA-approved IND protocol. The requirement for recordkeeping applies to IND vaccines,
antibiotics, and other medications in IND status.
7–4. Information requirements for investigational new drug products
Any recipient of an IND vaccine or chemoprophylaxis product must receive the information (for example, briefing,
individual counseling, information statements) required by the FDA-approved IND protocol. Full compliance with this
requirement is extremely important whether the IND product is voluntary or mandatory.
7–5. Coordination
The Army, as the Executive Agent for the Immunization Program for Biological Warfare Defense, maintains a program
office at the U.S. Army Medical Materiel Development Activity (USAMMDA) to execute oversight and coordination
of the use of IND products for Force Health Protection.
Chapter 8
Vaccines and Other Products Used Under Emergency Use Authorization
8–1. General
Under 21 USC 564 (The Food, Drug, and Cosmetic Act), some drugs, vaccines, or devices that have not been approved
or licensed by the FDA through the regular drug approval process (or not approved for an intended use) may be used
as medical countermeasures to chemical, biological, radiological, and nuclear (CBRN) agents or threats, if the FDA
grants an EUA. This EUA authority is an alternative to the otherwise applicable requirement to file an IND application
and follow IND rules (see chap. 7) to use such unapproved drugs as CBRN medical countermeasures.
8–2. Criteria
In general, the FDA may grant an EUA for up to 12 months, with potential renewal, based on the following:
a. The Secretary of Defense or designee has determined that there is a military emergency or significant potential
for a military emergency relating to a particular CBRN agent or threat.
b. The Secretary of DHHS declares an emergency based on the Secretary of Defense’s determination.
c. The Secretary of DHHS determines—
(1) The vaccine or drug may be effective in diagnosing, treating, or preventing the disease or condition.
(2) The known and potential benefits of the vaccine or drug outweigh the known and potential risks.
(3) There is no adequate, approved, and available alternative medical countermeasure.
d. The duration of authorization corresponds to the duration of the emergency or significant potential for an
emergency.
8–3. Refusal options
The FDA may decide that potential recipients of a drug under an EUA should have the option to refuse it. The
President may waive this option for military personnel.
8–4. Health recordkeeping requirements for emergency use authorization products
All EUA vaccines or chemoprophylaxis products that are administered must be recorded in the individual’s permanent
health record and/or DOD-approved electronic ITS.
8–5. Information requirements for emergency use authorization products
Any recipient of an EUA vaccine or chemoprophylaxis product must receive the information (for example, briefing,
individual counseling, information statements) required by the FDA-approved EUA. Full compliance with this require-
ment is critical.
8–6. Department of Defense requests for emergency use authorizations
Requests for possible EUAs for military purposes must be submitted to ASD (HA) for consideration.
8–7. Coordination
The Army, as the Executive Agent for the Immunization Program for Biological Warfare Defense, maintains a program
office at the USAMMDA. This office oversees and coordinates EUA product use for force health protection.
21AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Appendix A
References
Section I
Required Publications
Unless otherwise stated, all publications are available at: http://www.apd.army.mil/. Department of Defense regulations
are available at: http://www.dtic.mil/.
DODI 6200.03
Public Health Emergency Management within the Department of Defense (Cited in paras 3–3d, 3–6f.)
DODI 6205.4
Immunization of Other Than U.S. Forces (OTUSF) for Biological Warfare Defense (Cited in paras 3–3e, 3–6f.)
Section II
Related Publications
A related publication is a source of additional information. The user does not have to read a related publication to
understand this regulation. Unless otherwise stated, all publications are available at: http://www.apd.army.mil/. Depart-
ment of Defense regulations are available at: http://www.dtic.mil/. The U.S. Code and the Code of Federal Regulations
are available at: http://www.gpoaccess.gov/fdsys/.
AR 11–2
Managers’ Internal Control Program
AR 25–30
The Army Publishing Program
AR 600–20
Army Command Policy
AFI 48–123
Medical Examination and Standards (Available at http://www.e-publishing.af.mil/.)
Control of Communicable Diseases Manual
Communicable disease control and the international health regulations (Available at http://www.apha.org/.)
COMDTINST M6000.1
Medical Manual
DODD 1241.01
Reserve Component Medical Care and Incapacitation Pay for Line of Duty Conditions
DODD 1404.10
DOD Civilian Expeditionary Workforce
DODI 6200.02
Application of Food and Drug Administration (FDA) Rules to Department of Defense Force Health Protection
Programs
DODD 6205.02E
Policy and Program for Immunizations to Protect the Health of Service Members and Military Beneficiaries
DODD 6205.3
DOD Immunization Program for Biological Warfare Defense
DODI 1300.17
DOD Accommodation of Religious Practices Within the Military Services
DODI 1400.32
DOD Civilian Work Force Contingency and Emergency Planning Guidelines and Procedures
22 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
DODI 2310.08E
Medical Program Support for Detainee Operations
DODI 5010.40
Manager’s Internal Control (MCIP) Program Procedures
Executive Order 13139
Improving Health Protection of Military Personnel Participating in Particular Military Operations (Available at http://
www.archives.gov/federal-register/executive-orders/disposition.html/.)
NATO STANAG 2037
Vaccination of NATO Forces(Available at http://www.nato.int/docu/standard.htm/.)
NATO STANAG 2491
NBC/MED Policy for the Immunization of NATO Personnel Against Biological Warfare Agents(Available at http://
www.nato.int/docu/standard.htm/.)
NATO STANAG 3474
Temporary Flying Restrictions Due to Exogenous Factors Affecting Aircrew Efficiency (Available at http://www.nato.
int/docu/standard.htm/.)
10 USC 1107
Notice of use of an investigational new drug or a drug unapproved for its applied use
15 USC 1471
Definitions
15 USC 1472
Special packaging standards
15 USC 1473
Conventional packages, marketing
15 USC 1474
Regulations for special packing instructions
15 USC 1475
Repealed. Section 1205(c), Act of 13 August 1981, Public Law 97–35, Title XII, Volume 95, U.S. Statute at Large, p.
716.
15 USC 1476
Preemption of Federal standards
21 USC 360
Registration of producers of drugs or devices
42 USC 300aa
Public Health Service
42 USC 300aa–1 to 300aa–34
The National Childhood Vaccine Injury Act of 1986
42 USC 300aa–25
Recording and Reporting of Information
21 CFR 312
Investigational New Drug Application
29 CFR 1605
Guidelines on Discrimination Because of Religion
23AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
29 CFR 1910.1030.
Blood borne pathogens
Section III
Prescribed Forms
This section contains no entries.
Section IV
Referenced Forms
Except where otherwise indicated below, the following forms are available as follows: DA forms are available on the
APD Web site, at http://www.apd.army.mil; DD forms are available from the OSD Web site, at http://www.dtic.mil/
whs/directives/infomgt/forms/index.htm; standard forms (SFs) and optional forms (OFs) are available from the GSA
Web site (http://www.gsa.gov).
DA Form 11–2
Internal Control Evaluation Certification
DA Form 2028
Recommended Changes to Publications and Blank Forms
DD Form 2365
DOD Civilian Employee Overseas Emergency-Essential Position Agreement
DD Form 2766
Adult Preventive and Chronic Care Flowsheet (Available through normal forms supply channel.)
DD Form 2766C
Adult Preventive and Chronic Care Flowsheet (Continuation Sheet) (Available through normal forms supply channel.)
FDA Form 3500
MedWatch: The FDA Safety Information and Adverse Event Reporting System (Available at http://www.fda.gov/
Safety/MedWatch/default.htm).
Form VAERS–1
Vaccine Adverse Event Reporting System (Available at http://vaers.hhs.gov/esub/index)
CDC Form 731
International Certificate of Vaccination (Available through normal forms supply channel. Also available at http://
bookstore/gpo.gov, or toll free at 1-866-512-1800.) (Marine Corps and Navy - S/ N 0108–LF–400–0706. Available
from the Navy Supply System and may be requisitioned per NAVSUP P–2002D.)
SF 600
Medical Record - Chronological Record of Medical Care
SF 601
Health Record - Immunization Record
24 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Appendix B
Standards for Military Immunization
B–1. Standard #1: immunization availability
a. Ensure immunizations are available when required to minimize disruption of deployment or training schedules.
b. Ensure immunizations are available at convenient times, without unnecessary barriers and are available on a
walk-in basis, as staffing permits. As clinically appropriate, administer any vaccine doses required simultaneously to
avoid missed immunization opportunities.
c. Ensure immunization services are responsive to the needs of beneficiaries.
d. Review the vaccination status of all beneficiaries at every health care visit to determine which vaccines are
indicated.
e. Implement standing orders if written orders are unavailable. Standing orders must address vaccine dosage and
administration, contraindications and precautions, and documentation procedures. Ensure standing orders are signed by
the privileged physician who has medical oversight of the clinic.
B–2. Standard #2: vaccine information and vaccinee education
a. Educate beneficiaries about the benefits and risks of vaccination in a culturally appropriate manner and at an
appropriate education level.
b. Prior to vaccination, provide all parents/guardians and vaccinees the most current Vaccine Information Sheets
(VISs) for each vaccine as mandated by Federal law (42 USC 300aa-26). Allow sufficient time to discuss any concerns
or questions as noted by the vaccinee. Ensure VISs are accessible and visible in the patient waiting area of the clinic or
activity that provides immunizations.
c. Prior to each vaccination provide all potential vaccinees the opportunity to read the current DOD and/or FDA
mandated vaccine information brochure. Additional education requirements may be required as outlined in vaccination
policy.
d. Ensure immunization personnel are readily available to accurately answer patients’ immunization questions and
concerns about vaccines. Ensure personnel have ready access to immunization information resources.
B–3. Standard #3: vaccine storage and handling
a. Ensure staff members adhere to cold-chain management principles during administration, transportation, and
storage. Ensure up-to-date, written cold-chain management protocols are accessible at all locations where vaccines are
stored.
b. Implement temperature monitoring processes at any clinic or activity that administers immunizations. All vaccine
storage devices should have a calibrated thermometer and alarm systems that are visually monitored at a minimum of
twice a day.
c. The CDC’s National Center for Immunization and Respiratory Diseases strongly recommends that providers draw
vaccine only at the time of administration to ensure that the cold chain is maintained and that vaccine is not
inappropriately exposed to light. Do not pre-draw doses; draw them when they are needed.
B–4. Standard #4: indications and contraindications
a. Screen each patient for allergies, health status, recent vaccinations, and previous vaccine adverse events before
immunization. Provide each patient an opportunity to ask questions about potential contraindications. Refer patients for
appropriate medical evaluation, as needed.
b. Screen each patient’s immunization record to determine vaccine needs or requirements.
c. Ensure staff members document any contraindication to an immunization in the health record and ITS. Screen all
women for pregnancy status.
B–5. Standard #5: immunization recordkeeping
a. Record immunizations accurately in a DOD and USCG-approved electronic ITS according to Service-specific
policy at the time of immunization, or no later than 24 hours after administration of immunization. Transcribe all
historical immunizations into the immunization tracking system.
b. Recommend any clinic or activity that administers immunizations has one or more mechanisms for notifying
patients when the next dose of an immunization series is needed (a reminder system) or when doses are overdue (recall
system). Reminder and recall systems may be automated or manual and may include mailed, emailed, or telephone
messages.
c. Record all military personnel immunization information in an electronic ITS immunization record. All Services
must record military immunization data into an electronic database that communicates with a centralized DOD registry.
25AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
B–6. Standard #6: immunization personnel training
a. Ensure all persons who administer vaccines, including immunization augmentees, are appropriately trained and
work within their appropriate scope of practice as determined by Service policies.
b. Immunization training must meet a standard acceptable to the MTF commander, command surgeon, or other
appropriate medical authority. Training will include vaccine storage and handling; vaccine characteristics; recom-
mended vaccine schedules; patient screening; contraindications; vaccine administration techniques; and treatment and
reporting of adverse events to include anaphylaxis, vaccine benefit and risk communication, and documentation and
management.
c. Ensure personnel who administer vaccines complete a comprehensive immunization orientation and annual
continuing education that addresses training standards and competency of vaccine related topics based on an individu-
al’s role in administering and/or handling vaccines. Individuals who routinely administer vaccines should complete at
least 8 hours of training annually. Training resources include resident courses, self-paced online training programs, and
video training (see table B–1).
Table B–1
Training standards
Medical standard or procedure
Physicians and
medical directors
Immunizers Chapter and appendix
paragraph locations
Quality patient care and delivery of immunizations
Properly trained in accordance with DOD, Service, USCG, and
Centers for Disease Control and Prevention (CDC) guidelines
and act within their scope of practice as determined by each
Service.
B
1
, A
2
B, A 1–4c(1)
Understands standing order procedures for administering im-
munizations including dose, route, time indication, contrain-
dications, and so forth.
B, A B, A 2–1b and B–1
Demonstrates the ability and knowledge to screen individuals
for contraindications, hypersensitivities, allergies, and so forth,
before administering vaccines.
B B, A 2–1d and B–4
Understands and adheres to immunization dosing and interval
schedules.
B B, A 2–1e and B–6
Understands how to properly document exemptions from fur-
ther immunization in the ITS (DD Form 2766C), on the DD
Form 2766 (Adult Preventive and Chronic Care Flowsheet),
and/or in other relevant paper-based immunization records.
B B, A 2–6, 2–7, and B–4
Patient information and education before immunization
Understands the purpose of and legal requirements for making
VISs available to vaccine recipients.
B B, A 2–7d(2) and B–2
Understands how to document the date of the VIS in the ITS
when documenting an immunization given.
B B, A 2–7d(3) and B–2
Vaccine storage and handling
Trained in cold-chain management principles and procedures. B, A B, A 2–3 and B–3
Demonstrates how to read a vaccine package insert for stor-
age and handling requirements.
B B, A 2–3 and B–3
Understands proper reporting procedures for vaccine storage
and handling losses.
B, A B, A 2–3f and B–3
Emergency care and adverse-event reporting
Basic cardiopulmonary resuscitation and the administration of
epinephrine.
B, R
3
B, R 2–9b and B–6
Knows how to use the emergency equipment available for
treating an anaphylactic reaction. Ensures medications in kit
are not expired.
B B, A 2–9c and B–6
Demonstrates the ability to initiate anaphylactic reaction treat-
ments per protocol.
B B, A 2–9c and B–6
Understands the procedure for documenting an adverse event
after an immunization.
B B, A 2–10d and B–7
26 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Table B–1
Training standards—Continued
Knows how to submit a Vaccine Adverse Event Reporting
System (VAERS) Form 1.
B B, A 2–10d and B–7
Comprehends DOD’s Clinical Guidelines for Managing Ad-
verse Events after Immunization.
B, A B 2–10 and B–7
Understands how to handle and administer specific vaccines
Military and civilian personnel eligible to receive smallpox vac-
cine will be educated before immunization regarding criteria
for exemption from immunization, expected response at the
vaccination site, vaccination-site care, risks of spreading vac-
cinia to close contacts, and other relevant topics.
B, A B, A 4–15
Immunization record keeping (documentation)
Trained to accurately document immunizations, historical im-
munization data, and medical exception codes in ITS.
B B, A 2–6a and b, 2–7, and B–5
Training
Demonstrates understanding of and ability to follow this multi-
Service publication and other pertinent references such as
DOD, USCG, and CDC guidance in the performance of duties.
B, A B, A 1–5
Notes:
1
B=baseline or initial training
2
A=annually
3
R=as required
d. Ensure persons who administer vaccines have ready access to information resources regarding current recommen-
dations for childhood, general adult, travel, and military-specific immunizations.
B–7. Standard #7: adverse events after immunization
a. Epinephrine (such as auto-injectable epinephrine) must be properly stored and readily available at all vaccination
locations along with other supplies determined locally to manage adverse events (see para 2–9). Ensure all immuniza-
tion personnel are trained to administer epinephrine.
b. Provide easy access to telephones or radios to persons who administer vaccines for summoning emergency
medical personnel. Medical providers document adverse events in the health record at the time of the event or as soon
as possible thereafter.
c. Report all clinically significant adverse events after vaccination to VAERS. Provide staff members with ready
access to reporting options for the VAERS.
d. Develop a quality improvement process to assure adverse events are reported to VAERS promptly.
B–8. Standard #8: vaccine advocacy to protect the military Family
a. Develop a mechanism at the MTF level to determine the extent of influenza and pneumococcal immunization
coverage among its high-risk patients. Develop a plan to optimize vaccination uptake and coverage.
b. Implement a plan to optimize immunization rates among cardiac, pulmonary, diabetic, asplenic, and other patient
groups at elevated risk of complications from vaccine-preventable infectious diseases.
c. Conduct a quality improvement program to optimize the performance in immunizing children, adolescents, and
adults against the preventable infections that most threaten them.
d. Ensure commanders use immunization databases to identify and resolve the vulnerabilities of their units.
e. All health care providers (not just those in any clinic or activity that administers immunizations) should routinely
determine the immunization status of their patients, offer vaccines to those for whom they are indicated, and maintain
complete immunization records.
27AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Appendix C
Medical and Administrative Exemption Codes
This appendix gives details about medical and administrative exemption codes, as well as information on duration.
C–1. Medical exemption codes
Medical exemption codes appear in table C–1.
Table C–1
Medical exemption codes
Code Meaning Explanation of example Duration
MD Medical, declined Declination of optional vaccines (not applicable to military required vacci-
nations).
Indefinite
MA Medical, assumed Prior immunization reasonably inferred from individual’s past experiences
(for example, basic military training), but documentation missing. Code
used to avoid superfluous immunization. Code can be reversed upon fur-
ther review.
Indefinite
MI Medical, immune Evidence of immunity (for example, by serologic antibody test ); docu-
mented previous infection (for example, chickenpox infection); natural in-
fection presumed (for example, measles, if born before 1957).
Indefinite
MP Medical, perma-
nent
HIV infection, prolonged or permanent immune suppression, upper age
limit, other contraindication determined by physician. Can be reversed if
the condition changes. For tuberculosis, positive tuberculosis test.
Indefinite
MR Medical, reactive Permanent restriction from receiving additional doses of a specific vaccine.
Use only after severe reaction after vaccination (for example, anaphylaxis).
Report such reactions to VAERS. Code can be reversed if an alternate
form of prophylaxis is available. Do not code mild, transient reactions as
MR. code events referred for medical consultation as MT.
Indefinite
MS Medical, supply Exempt due to lack of vaccine supply. Up to 90 days
MT Medical, tempo-
rary
Pregnancy, hospitalization, events referred for medical consultation, tem-
porary immune suppression, convalescent leave, pending medical evalua-
tion board, any temporary contraindication to immunization.
Up to 365 days
C–2. Administrative exemption codes
Administrative exemption codes appear in table C–2.
Table C–2
Administrative exemption codes
Code Meaning Explanation of example Duration
AD Administrative, deceased Individual is deceased. Indefinite
AL Administrative, emergency leave Individual is on emergency leave. Up to 30 days
AM Administrative, missing Missing in action, prisoner of war. Indefinite
AP Administrative, PCS Permanent change of station. Up to 90 days
AR Administrative, refusal Personnel involved in actions under the Uniformed Code of
Military Justice, religious waiver. (Indefinite and revocable.
May be revoked at any time. See paragraph 2–6b(2.
Until resolution
AS Administrative, separation Pending discharge, separation (typically within 60 days), and
retirement (typically within 180 days).
Until 180 days
AT Administrative, temporary Absent without leave, legal action pending (other than code
AR).
Until 90 days
NR Not required Individuals who received immunization while eligible, sub-
sequently changed occupational category and now serve as
civilian employees or contract workers not otherwise required
to be immunized.
Indefinite
28 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
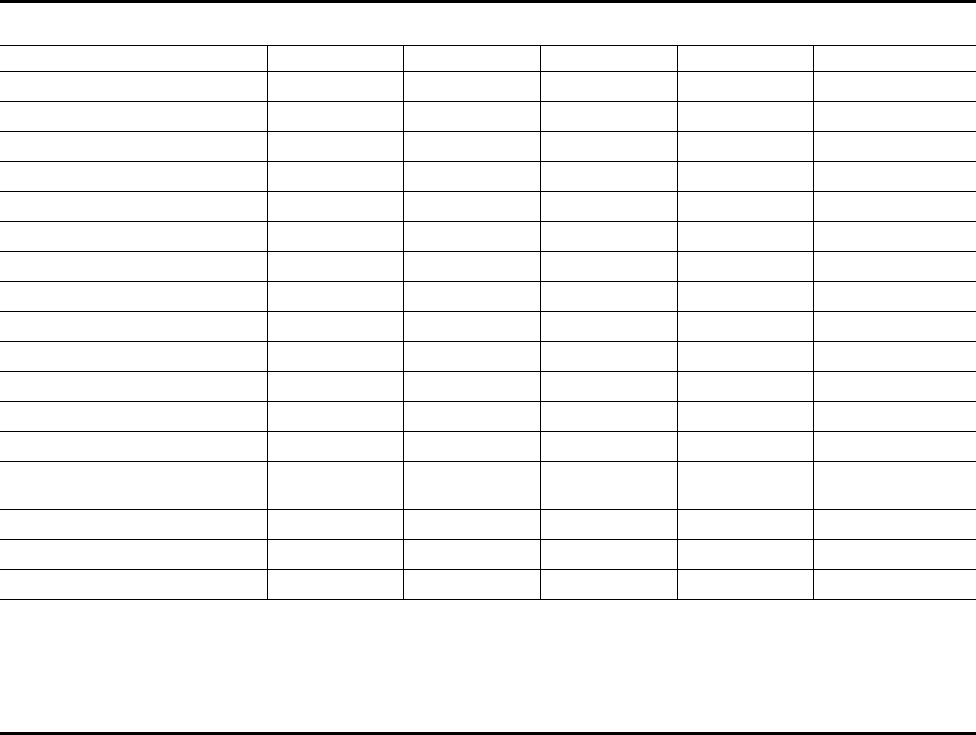
Appendix D
Immunizations for Military Personnel
D–1. Text citations
Paragraphs 4–2 to 4–19 provide additional information on immunizations for military personnel.
D–2. Required immunizations
This table provides a listing of required immunizations for military personnel.
Table D–1
Immunizations for military personnel
Name of vaccine Army Navy Air Force Marine Corps Coast Guard
Adenovirus
1
Acc
2
Acc Acc Acc Acc
Anthrax Risk Risk Risk Risk Risk
Haemophilus influenzae type b Risk Risk Risk Risk Risk
Hepatitis A Acc, Rou
3
Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Hepatitis B Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Influenza Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Japanese encephalitis Risk
4
Risk Risk Risk Risk
Measles, mumps, rubella Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Meningococcal Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Pneumococcal Risk Risk Risk Risk Risk
Poliovirus
5
Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Rabies Risk Risk Risk Risk Risk
Smallpox (vaccinia) Risk Risk Risk Risk Risk
Tetanus-diphtheria (preferably with
pertussis vaccine)
Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Typhoid fever Risk Risk Risk Risk Risk
Varicella Acc, Rou Acc, Rou Acc, Rou Acc, Rou Acc, Rou
Yellow fever Risk Risk Risk Acc, Risk Risk
Notes:
1
Initial entry and basic training accessions only
2
Acc=accessions
3
Rou=adult routine
4
Risk=special, risk-based, and occupational
5
Refer to paragraph 4–13.
29AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Appendix E
Internal Control Evaluation Process
E–1. Function
The function covered by this checklist is immunization and chemoprophylaxis.
E–2. Purpose
The purpose of this checklist is to assist in evaluating key management controls and is not intended to address all
controls. The evaluation is focused at the clinic level, regardless of Service, to include both fixed facilities (MTFs,
TDA units) and TOE field units. The checklist serves as a clinical quality improvement tool and is described at http://
www.vaccines.mil/cqiip.
E–3. Instructions
Answers must be based on the actual testing of key management controls (for example, document analysis, direct
observation, interviewing, sampling, or simulation). Answers that indicate deficiencies must be explained and correc-
tive action indicated in supporting documentation. These key management controls must be formally evaluated at least
once every 5 years. Certification that this evaluation has been conducted must be accomplished on DA Form 11–2–5
(Internal Control Evaluation Certification Statement).
E–4. Test questions
Test questions are available directly via a link at the Web site address in paragraph E–2, above.
E–5. Supersession
This evaluation replaces the evaluation for immunization and chemoprophylaxis previously published in AR 40–562,
dated 29 September 2006.
30 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Glossary
Section I
Abbreviations
ACIP
Advisory Committee on Immunization Practices
AFI
Air Force Instruction
AFJI
Air Force Joint Instruction
ASD (HA)
Assistant Secretary of Defense (Health Affairs)
CBRN
chemical, biological, radiological, and nuclear
CDC
Centers for Disease Control and Prevention
CFR
Code of Federal Regulations
CG–11
Coast Guard, Director, Health, Safety, and Work-Life
COMDTINST
Commandant Instructions
DCJI
disposable-cartridge jet injectors
DD
Department of Defense Form
DHHS
Department of Health and Human Services
DODD
Department of Defense Directive
DODI
Department of Defense Instruction
EUA
emergency use authorization
FDA
Food and Drug Administration
G6PD
glucose-6-phosphate dehydrogenase
Hib
Haemophilus influenzae type b
HQ
headquarters
31AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
HQDA
Headquarters, Department of the Army
IND
investigational new drug
IPV
inactivated poliovirus vaccine
ITS
immunization tracking systems
JTF CapMed
Joint Task Force - National Capital Region/Medical
JEV
Japanese-encephalitis vaccine
MAJCOM
major command (Air Force)
MILVAX
Military Vaccine Office
MMR
measles, mumps, rubella
MTF
medical treatment facility
NCVIA
National Childhood Vaccine Injury Act
NVIC
National Vaccine Injury Compensation (Program)
OTUSF
other than U.S. Forces
RC
reserve component
ROTC
Reserve Officers’ Training Corps
SF
Standard Form
SOP
standard operating procedure
SSN
social security number
STANAG
standardized agreement
TB
tuberculosis
32 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Td
Tetanus-diphtheria
Tdap
Tetanus-diphtheria and acellular pertussis (vaccine)
USAMMDA
U.S. Army Medical Materiel Development Activity
USC
United States Code
USCG
United States Coast Guard
VAERS
Vaccine Adverse Events Reporting System
VIS
vaccine information statement
WHO
World Health Organization
Section II
Terms
This section contains no entries.
Section III
Special Abbreviations and Terms
Accession
The attainment of rank or dignity.
Alert personnel
Specified forces maintained (alert force) in a special degree of readiness.
Antigen
A substance that, when introduced into the body, stimulates the production of an antibody.
Contraindication
A factor that renders the administration of a drug or the carrying out of a medical procedure inadvisable.
Hyperendemic
Equally endemic, at a high level, in all age groups of a population.
Neisseria meningitides
The bacteria that is the causative agent of cerebrospinal meningitis.
Plasmodia
A genus of apicomplexan protozoa, in the family Plasmodiidae parasitic, in the blood cells of animals and humans; the
malarial parasite.
Primaquine
An ant malarial agent especially effective against Plasmodium vivax.
Seroimmunity
Immunity conferred by administration of an antiserum.
33AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
Serologic
The scientific study of blood serum and other bodily fluids.
Toxoid
A bacterial toxin (usually an exotoxin) whose toxicity has been weakened or suppressed either by chemical (formalin)
or heat treatment, while other properties, typically immunogenicity, are maintained.
Urticaria
A skin condition characterized by intensely itching welts and caused by allergic reactions.
Variola virus
The causative agent of smallpox.
34 AR 40–562/BUMEDINST 6230.15B/AFI 48–110_IP/CG COMDTINST M6230.4G • 7 October 2013
UNCLASSIFIED PIN 000011–000
