
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 1 of 52
Medicaid Transportation
Policy Manual
New York State Medicaid Transportation Provider
Policy Manual
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 2 of 52
Table of Contents
1 Definitions
3
2 Generals Requirements and Background 9
2.1 Transportation Populations and Coverage 9
2.2 New York State Medicaid Transportation Services 11
2.3 Prior Authorization 12
2.4 Transportation Provider Requirements and Responsibilities 17
2.5 Record Keeping Requirements and Reporting 21
2.6 Complaints and Complaints Reporting 25
2.7 Claims and Reimbursement 25
3 Specific Minimum Qualifications by Category of Service 32
3.1 Ambulance Providers – Category of Service 0601 32
3.2 Ambulette Providers – Category of Service 0602 41
3.3 Taxi (Category of Service 0603) and NYC Livery (Category of Service 0605) Providers 48
3.4 Transportation Network Companies (TNC) – Category of Service 0609 Providers 49
4 Document Control Properties 49
Appendix 1 – Ambulance Service and Advanced Life Support Form 50
Appendix 2 – Acceptable Claim Modifiers 51
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 3 of 52
1. Definitions
For the purposes of the Medicaid program, and as used in this Manual, the following terms are
defined.
Advanced Life Support Services
Advanced life support (ALS) services are those ambulance services in which the treatment
provided is invasive to the patient, or above the level of care provided that can be provided by a
NYS Certified Emergency Medical Technician-Basic. Such invasive treatment may include but
not be limited to:
• Advanced Prehospital patient assessment
• The initiation and monitoring of intravenous (IV) fluids
• Cardiac monitoring (ECG)
• Intubation/insertion of an airway tube, manual ventilations or the monitoring of an
electronic ventilation device
• Manual defibrillation and/electric pacing of the patient’s heart
• Administration or monitoring of most medications given by mouth, injection or IV drip, and
• Communication with a physician and the transmission of patient data, such as ECG
From Public Health Law, Article 30, §3001(11) – “Advanced life support care means definitive
acute medical care provided, under medical control, by advanced emergency medical
technicians within an advanced life support system.” Such advanced life support care must be
provided in accordance with the New York State Department of Health Collaborative Advanced
Life Support Adult and Pediatric Treatment Protocols.
https://www.health.ny.gov/professionals/ems/docs/collaborative_protocols.pdf
Advanced Life Support Assistance
An advanced life support assist is an emergency ALS response, in conjunction with an
emergency ambulance transport provided by another, basic life support (BLS) ambulance
service.
It this type of response, an ambulance service, or advanced life support first response service,
is dispatched to an emergency medical call, to assist the primary BLS ambulance service, by
providing medical necessary ALS services, which the primary BLS ambulance service is not
authorized to provide. Please see further on in this manual for reimbursement in such situations.
Advance Life Support First Response Service
Advanced life support first response service means an organization which provides advanced
life support care but does not transport patients.
Adult Day Health Care
Adult Day Health Care (ADHC) programs are community-based programs licensed by the New
York State Department of Health which provide comprehensive medically supervised care in a
congregate setting to individuals with a physical or mental impairment.
https://www.health.ny.gov/health_care/medicaid/program/longterm/addc.htm
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 4 of 52
Ambulance (Category of Service 0601)
Ambulance means a motor vehicle, aircraft, boat, or other form of transportation designed and
equipped to provide emergency medical services during transit.
Ambulance Service
Ambulance Service means any entity, as defined in Section 3001 of the Public Health Law,
which is engaged in the provision of emergency medical services and the transportation of sick,
disabled, or injured persons by motor vehicle, aircraft, boat or other form of transportation to or
from facilities providing hospital services and which is currently certified or registered by the
NYS Department of Health (NYSDOH or The Department) as an ambulance service.
https://www.health.ny.gov/professionals/ems/policy/06-06.htm
Ambulette (Category of Service (0602)
Ambulette or paratransit vehicle means a special-purpose vehicle, designed and equipped to
provide nonemergency transport, that has wheelchair-carrying capacity, stretcher-carrying
capacity, or the ability to carry disabled individuals.
Basic Life Support Services
Basic Life Support (BLS) services are ambulance services in which the treatment provided to
the patient is within the scope of practice for a NYS-certified EMT Basic, and in accordance with
the New York State Department of Health Statewide Pre-Hospital Treatment Protocols
bls_protocols.pdf (ny.gov)
Common Medical Marketing Area (CMMA)
The common medical marketing area is the geographic area from which a community,
customarily obtains its medical care and services.
Community
A community is either the State, or a portion of the State, a city or particular classification of the
population, such as all persons 65 years of age and older.
Conditional Liability
Conditional Liability is the responsibility of the prior authorization official for making payment
only for transportation services which are provided to a Medical-eligible individual in accordance
with the requirements of Title 18 NYCRR.
Day Treatment Program or Continuing Treatment Program
A day treatment program or continuing treatment program is a planned combination of
diagnostic, treatment and rehabilitative services offered by the Office for People with
Developmental Disabilities (OPWDD) or the Office of Mental Health (OMH).
Department-Established Reimbursement Fee
A Department-established fee is the fee for any given mode of transportation that the
Department has determined will ensure the efficient provision of appropriate transportation to
Medicaid enrollees in order for the enrollee to obtain necessary medical care or services.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 5 of 52
Emergency Ambulance Transportation
Emergency ambulance transportation means the provision of ambulance transportation for the
purpose of obtaining hospital services for a Medicaid enrollee who suffers from severe, life-
threatening or potentially disabling conditions, which require the provision of emergency medical
services while the enrollee is being transported.
Emergency Medical Services
Emergency Medical Services are services for the provision of initial, urgent medical care
including, but not limited to, the treatment of trauma, burns, and respiratory, circulatory and
obstetrical emergencies.
Emergency triage, treat and transport (ET3) model
Emergency triage, treat, and transport (ET3) model means an innovative payment and service
delivery model established by the United States Department of Health and Human Services to
lower costs and improve quality of care to Medicare enrollees by requiring ambulance service
suppliers selected by the Center for Medicare and Medicaid Innovation (CMMI), or successor
agency or office, to partner with qualified health care practitioners to deliver treatment in place
and/or transport to alternative destination sites, such as primary care physician offices, urgent
care centers, federally qualified health centers, and mental health or substance use disorder
crisis centers.
On or after November 24, 2021, and subject to federal financial participation, Medicaid
payments will be made to ambulance service vendors that participate in an ET3 model as
follows:
In order to participate in this model for Medicaid payment purposes, an ambulance service
provider shall submit:
1. A copy of its ET3 application as submitted to CMMI;
2. A copy of the approval letter from CMMI; and,
3. Any other documentation deemed necessary by the Department to confirm Medicare ET3
payments are being made to the vendor
The Department established fees for services provided under an ET3 model, which may
include value-based payments, shall be fore:
1. Transport to an alternative non-hospital destination, a base fee plus a mileage charge;
and
2. Treatment in place without transport, a base fee without a mileage charge.
3. Ambulance service vendors receiving Medicaid payments in accordance with this
subdivision shall submit to the Department copies of all reports provided to CMMI during
the course of the Medicare demonstration.
4. Medicaid payments under the ET3 model will continue only for the duration of the
Medicare demonstration approved by CMMI and will be terminated when either the
demonstration period expires or upon termination of Medicare participation by CMMI at
any time for any reason.
Please Note: The Centers for Medicare and Medicaid Services has decided to end ET3 as
of December 31, 2023, due to lower than expected participation and lower than projected
interventions. https://innovation.cms.gov/innovation-models/et3
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 6 of 52
Livery Vehicles (Category of Service 0605)
Livery Vehicles are defined in New York State Department of Motor Vehicles and Traffic Law
Article 1 § 121-e. as every motor vehicle, other than a taxicab or a bus, used in the business of
transportation passengers for compensation. However, it shall not include vehicles which are
rented or leased without a driver. This category of service is a curb to curb service, is exclusive
to NYC and requires proper taxi/limousine commission licensure.
Local Departments of Social Services
The Local Department of Social Services (LDSS) is the locality that authorizes a Medicaid
enrollee’s eligibility for Medicaid for all counties outside of New York City. The Human
Resources Association (HRA) authorizes a Medicaid enrollee’s eligibility for Medicaid in the 5
boroughs of New York City. There are sixty (60) LDSS in New York State, including the five (5)
boroughs encompassing New York City, as well as both the New York State OMH and the
OPWDD.
Locally Established Fee
Locally established fee means the fee for any given mode of transportation which the
Transportation Broker has determined will ensure the efficient provision of appropriate
transportation for Medicaid enrollees in order for the enrollees to obtain necessary medical care
or services.
Locally Prevailing Fee
Locally prevailing fee means a fee for a given mode of transportation which is established by a
transit or transportation authority, or commission empowered to establish fees for public
transportation, a municipality, or a third-party payor, and which is charged to all persons using
that mode of transportation in a given community.
New York State Office of Mental Health (OMH) and the Office for People with Developmental
Disabilities (OPWDD)
OMH and OPWDD are two State agencies operating as local departments of social services in
New York State. Upon eligibility verification, OMH is represented by county code 97 and
OPWDD by county code 98. The Department’s prior authorization official (transportation broker)
shall be responsible for the prior authorization of both emergency and non-emergency medical
transportation services for enrollees assigned to them.
Non-Emergency Ambulance Transportation
Non-emergency ambulance transportation means the provision of ambulance transportation for
the purpose of obtaining necessary medical care or services to a Medicaid enrollee whose
medical condition requires transportation by an ambulance service.
New York State Medicaid Payment System
New York State Medicaid payment system means an automated system, such as eMedNY,
used to process Medicaid fee-for-service claims submitted by Medicaid enrolled providers for
services provided to Medicaid enrollees.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 7 of 52
Ordering Practitioner
Ordering practitioner means the Medicaid enrollee’s attending physician or other medical
practitioners, who has not been excluded from enrollment in the Medicaid program, and who is
requesting transportation on behalf of the Medicaid enrollee so that the Medicaid enrollee may
obtain medical care or services which are covered under the Medicaid program. The ordering
practitioner is responsible for initially determining when a specific mode of transportation to a
particular medical care of service is medically necessary.
Personal Assistance
Personal Assistance means the provision of physical assistance by a provider of transportation
services to a Medicaid enrollee for the purpose of assuring safe access to and from the
enrollee’s place of residence, the transportation provider’s vehicle, and the Medicaid-covered
health service provider’s place of business. Personal assistance is the rendering of physical
assistance to the enrollee to enable walking, climbing or descending stairs, ramps, curbs, or
other obstacles; opening or closing doors; accessing a vehicle; and the moving of wheelchairs
or other items of medical equipment and the removal of obstacles as necessary to assure the
safe movement of the enrollee. In providing personal assistance, the provider or the provider’s
employee will physically assist the enrollee which shall include touching, or, if the enrollee
prefers not to be touched, guiding the enrollee in such close proximity that the provider of
services will be able to prevent any potential injury due to a sudden loss of steadiness or
balance. An enrollee who can walk to and from a vehicle to their home and place of medical
services without such assistance is deemed not to require personal assistance.
Prior Authorization/Prior Approval
Prior authorization means a prior authorization official’s determination that payment for a
specific mode of transportation is essential in order for a Medicaid enrollee to obtain necessary
medical care and services and that the prior authorization official accepts conditional liability for
payment of the enrollee’s transportation costs.
Prior Authorization Number
The 11-digit number obtained by the transportation provider through the transportation broker,
or available through the NYS DOH MMIS system. The transportation provider uses this number
to complete claims for payment in eMedNY.
Prior Authorization Official
Prior authorization official means the Department, the transportation broker, or such other entity
under contract with, or specifically permitted by, the Department of Health, as applicable.
Provider Network
The Transportation Broker’s established collection of transportation providers used to complete
non-emergency medical transportation trips for NYS Medicaid members. The network providers
must sign a network service agreement with the Transportation Broker and be Medicaid
enrolled.
Service Agreement
Service Agreement means an agreement between a vendor and a transportation broker that
includes, but is not limited to, vendor service standards and fees to be established for the
provision of non-emergency transportation services to Medicaid enrollees.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 8 of 52
Service Animal
Service animals are defined as dogs that are individually trained to do work or perform tasks for
people with disabilities. Examples of such work or tasks include guiding people who are blind,
alerting people who are deaf, pulling a wheelchair, alerting and protecting a person who is
having a seizure, reminding a person with mental illness to take prescribed medications,
calming a person with Post Traumatic Stress Disorder (PTSD) during an anxiety attack, or
performing other duties. Services animals are working animals, not pets. The work or task a dog
has been trained to provide must be directly related to the person’s disability. Dogs whose sole
function is to provide comfort or emotional support do not qualify as service animals under the
ADA. ADA Information and NYS Information.
Stretcher Ambulette (Category of Services 0602)
Stretcher service is considered non-emergency transportation of a Medicaid enrollee who must
be transported to and from medical care, is confined to bed, cannot sit in a wheelchair, and
does not require medical attention/monitoring during transport. These transports are normally
completed in a retro fitted ambulette vehicle.
Taxicab (Category of Service 0603)
Taxi vehicles are defined in New York State Department of Motor Vehicle and Traffic Law (VTL)
Article 1, §148-a. as every motor vehicle, other than a bus, used in the business of transporting
passengers for compensation, and operated in such business under a license of permit issued
by a local authority. However, it shall not include vehicles which are rented or leased without a
driver. Taxicab is a curb to curb service.
Trip Attestation
Trip attestation is defined as the confirmation that a trip has been completed by the
transportation provider. The transportation provider is required to follow any system or
communication procedures defined by the transportation broker to attest that a trip has been
completed. Trip attestation is required to receive a prior authorization number and to submit a
claim for payment.
Transportation Attendant
Transportation Attendant is any individual authorized by the prior authorization official to
accompany and assist the Medicaid enrollee in receiving safe transportation.
Transportation Brokers
Transportation management broker(s) or transportation broker(s) means the entity or entities
with which the commissioner contracts to cost-effectively administer non-emergency
transportation services to Medicaid enrollees in accordance with Social Services Law section
365-h(4)(b).
Transportation Network Company TNC (Category of Service 0609)
Transportation Network Company or TNC means a person, corporation, partnership, sole
proprietorship, or other entity that is licensed pursuant to Vehicle and Traffic Law Chapter 71
Title 8 Article 44-B Section 1691 and is operating in New York State exclusively using a digital
network to connect transportation network company passenger to transportation network

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 9 of 52
company drivers who provide TNC prearranged trips.
https://www.nysenate.gov/legislation/laws/VAT/1691
Transportation Services
Transportation services means:
1. Transportation by public transit, self-drive mileage reimbursement, ambulance,
ambulette, or paratransit vehicle, taxicab/livery, transportation network company/high-
volume for-hire services vehicle (TNC), common carrier, or other means appropriate to
the Medicaid enrollee’s medical condition’ and
2. A transportation attendant to accompany the Medicaid enrollee, if necessary. Such
services may include the transportation attendant’s transportation, meals, lodging and
salary, however, salary will not be paid to a transportation attendant who is a member of
the Medicaid enrollee’s family.
Undue Financial Hardship
Undue financial hardship means transportation expenses which the Medicaid enrollee cannot
be expected to meet from monthly income or from available resources. Such transportation
expenses may include those of a recurring nature or major one-time costs.
Value-based payment
Value-based payment means an additional fee for certain transportation services determined by
the Department that may be paid to vendors that achieve certain quality and/or efficiency targets
established by the Department or a transportation broker.
Vendor
Vendor means a lawfully authorized provider of transportation services who is enrolled in the
Medicaid program pursuant to Part 504 of this Title and authorized to receive payment for
transportation services directly from the New York State Medicaid payment system or pursuant
to a service agreement with a transportation management broker, as applicable. The term
vendor does not mean a Medicaid enrollee or another individual who transports a Medicaid
enrollee by means of a private vehicle.
Wheelchair
A manually operated or power-driven device designed primarily for use by an individual with a
mobility disability for the main purpose of indoor or of both indoor and outdoor locomotion.
2. General Requirements and Background
2.1 Transportation Populations and Coverage
Both emergency and non-emergency medical transportation are benefits covered by the New
York State Medicaid program. Emergency medical transportation is always provided by
ambulance providers.
Non-emergency medical transportation (NEMT) is an important benefit for enrollees who need
to get to and from medical services but have no means of transportation. The Code of Federal
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 10 of 52
Regulations [42 CFR § 440.170(a)] requires States to ensure that eligible, qualified Medicaid
enrollees have NEMT to take them to and from medical providers.
https://www.cms.gov/medicare-medicaid-coordination/fraud-prevention/medicaid-integrity-
education/downloads/nemt-booklet.pdf
Medicaid Managed Care Involvement
One of the Medicaid Redesign Team’s (MRT) Transportation Reform initiatives was the
carveout of transportation from the Medicaid (mainstream) Managed Care benefit package. The
non-emergency transportation of mainstream managed care enrollees transitioned to the
Department’s contracted Medicaid transportation managers/broker on December 1, 2015.
Sources: October 2015 Medicaid Update; August 2015 Medicaid Update
However, some Managed Care Plans (also referred to as Prepaid Capitation Plans or Medicaid
Health Maintenance Organizations) currently include transportation (emergency, non-emergency
or both emergency and non-emergency) within their scope of benefits. Covered services are
identified in the eligibility verification process. For more information, please consult the Medicaid
Eligibility Verification System (MEVS) Manual, online at:
https://www.emedny.org/ProviderManuals/AllProviders/supplemental.aspx
For enrollees covered by plans that include transportation as a covered benefit, claims coming to
Medicaid for the transportation of such enrollees will be denied. The provider must contact the
Managed Care Plan for reimbursement.
Questions concerning Medicaid eligibility verification should be addressed to the eMedNY Call
Center at (800) 343-9000.
Managed Long Term Care Involvement
The Department is transitioning to a Transportation Management Broker. Beginning in 2024,
the Department will begin “carving out” transportation from the Managed Long Term Care
benefit. The “carve out” will be phased in over several months.
Transportation Under the Family Planning Benefit Program
Effective November 1, 2012, the Family Planning Benefit Program (FPBP) includes
transportation of eligible enrollees to family planning services covered by the FPBP.
Source: November 2012 Medicaid Update
Programs and Facilities Certified by the OPWDD
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 11 of 52
OPWDD Day Treatment, Day Habilitation, Community Habilitation, Prevocational Services, and
Employment Services agencies must provide or pay for transportation to and from their
programs using their day program reimbursement.
OPWDD certified Intermediate Care Facilities (ICF/DDs), Supervised Community Residences,
and Supervised and Supportive Individualized Residential Alternatives must provide or pay for all
resident transportation to medical and clinical appointments at no additional cost to the
Medicaid program. Ambulance services should not be utilized for routine transportation to
medical or clinical visits, or to and from day programs. Emergency (911-generated) ambulance
services, or ambulance discharge from a hospital, may be billed separately to the Medicaid
Program on a fee-for-service basis.
Adult Day Health Care (ADHC) Transportation
Many ADHC programs either contract separately with Medicaid-enrolled transportation providers
or own vehicles to transport registrants to and from the program. In these cases, the ADHC,
not the Medicaid program, reimburses the transportation provider directly. Prior authorization
for transportation of registrants to and from such programs, excluding transportation for ad hoc
medical appointments that take place on the same date as an ADHC visit, will not be granted.
2.2 New York State Medicaid Transportation Services
Medicaid reimbursement is available to lawfully authorized transportation providers for
transportation furnished to eligible Medicaid enrollees when necessary to obtain medical care
covered by the Medicaid program. Payments for transportation services are limited to the
provision of Medicaid enrollee passenger-occupied transportation to or from Medicaid-covered
services.
The Medicaid program must assure that necessary transportation is available to Medicaid
enrollees.
This assurance requirement means that Medicaid will consider assisting with the costs of
transportation when the costs of transportation become a barrier to accessing necessary
medical care and services covered under the Medicaid program. The decision to assist with the
costs of transportation is called the “prior authorization process.”
Emergency ambulance transportation does not require prior authorization. All other modes of
transportation, while available to a Medicaid enrollee, must be prior authorized by the
appropriate prior authorization official prior to payment by the Medicaid program.
Approved requests for prior authorization are communicated to the transportation provider.
Approved prior authorization numbers are necessary to submit a valid claim to the Medicaid
program. The information on the claim must match the information on the prior authorization as
one condition for the claim to be paid.
Non-emergency transportation services may include the following modes of transportation:
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 12 of 52
• Ambulance (ground and air);
• Ambulette (wheelchair van or van with stretcher-carrying capacity); and
• Taxi/livery
• Rideshare/Transportation network company (TNC)
• Public Transportation
• Mileage reimbursement
The Medicaid program shall authorize transports using the most cost effective, medically-
appropriate mode of transport. If a Medicaid enrollee uses the public transit system for the
activities of daily life, then, in most circumstances, transportation for the enrollee should be
requested at a mode of transportation no higher than that of the public transit system.
The mode of transportation used by a Medicaid enrollee must be decided by a medical
practitioner who is directly involved in the patient’s care, and therefore, best situated and
qualified to determine the most appropriate mode.
All Medicaid medical transportation must be in accordance with Department regulation at Title
18 of the New York Code of Rules and Regulations (NYCRR) Section 505.10
https://regs.health.ny.gov/volume-c-title-18/content/section-50510-transportation-medical-care-
and-services
In addition to all State requirements, 42CFR §1902(a)(87) requires that all State Medicaid
plans must include certain minimum requirements.
These federal minimum requirements under the state plan must include that:
(A) Each provider and individual driver are not excluded from participation in any federal
health care program (as defined in section 1128B(f) of the Act) and is not listed on the
exclusion list of the Inspector General of the Department of Health and Human Services;
(B) Each such individual driver has a valid driver’s license;
(C) Each such provider has in place a process to address any violation of a state drug law;
and
(D) Each such provider has in place a process to disclose to the state Medicaid program, the
driving history, including any traffic violations, of each such individual driver employed by
such provider..
https://www.medicaid.gov/federal-policy-guidance/downloads/cib071221.pdf
2.3 Prior Authorization
Prior Authorization Process
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 13 of 52
Payment will not be made for non-emergency transports if the transportation provider does not
receive authorization for the transport.
Prior authorization must be obtained from the applicable prior authorization official as identified in
section 2.3.
To determine the appropriate procedures, please consult the transportation broker identified in
the eligibility verification process using the contact list available online at:
http://www.emedny.org/ProviderManuals/Transportation/index.html
In most instances, approval must be obtained prior to each trip (or round trip) taken by the
Medicaid enrollee. If a Medicaid enrollee requires regular transportation due to extended
treatment (such as dialysis) and the enrollee’s medical appointment is at the same location, and
if the same provider is to transport the enrollee, a standing order prior approval may be granted
for an extended period. Whenever such prior authorization for non-emergency transportation is
not obtained, reimbursement will be denied.
Any changes to trip details, such as location, and/or day, must be approved by the prior
authorization official prior to providing the service. Failure to do this may result in non-payment.
Prior authorization does not guarantee payment. Unmet provider and enrollee eligibility
requirements may result in the denial of reimbursement. Comprehensive billing information can
be found in the Billing Guidelines Manual, available online at:
http://www.emedny.org/ProviderManuals/Transportation/index.html
NYSDOH-Contracted Prior Authorization Official
The NYSDOH has contracted with professional transportation management entities to manage
transportation on behalf of Medicaid enrollees.
Effective on or after August 1, 2023, based on a competitive procurement, non-emergency
medical transportation will be transitioned by the State from the current Medicaid Transportation
managers to one Medicaid Transportation Broker (Medical Answering Services, LLC or MAS)
to ensure that Medicaid eligible individuals receive reliable, high quality NEMT services using
the mode that is appropriate for each individual. MAS will assume Medicaid Transportation
Broker responsibilities for all counties except Nassau and Suffolk on August 1, 2023. Nassau
and Suffolk counties will transition to MAS for all Medicaid Transportation Broker responsibilities
on December 1, 2023. The Medicaid Transportation Broker will contract directly with
transportation providers to develop an adequate network, ensure compliance with transportation
network driver and vehicle requirements, and negotiate fee-for-service transportation provider
reimbursement.
The NYSDOH-contracted transportation broker has no vehicles and will not provide
transportation in competition with existing Medicaid-enrolled transportation vendors.
Transportation vendors will need to agree to and sign a service agreement with the
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 14 of 52
transportation broker in order to participate in their transportation network and receive
trip assignments. Medicaid enrollment does not guarantee acceptance in the
transportation broker’s provider network. The transportation broker is allowed to utilize all
transportation vendors who participate in their network, to whatever extent determined by the
transportation broker.
The Department expects that transportation vendors will adhere to the Department's standards
concerning trip reroutes, i.e., if a trip cannot be accommodated, the vendor will notify the
transportation broker as required.
Through this contract with NYSDOH, the transportation broker is primarily tasked with:
• accepting requests for non-emergency Medicaid-funded transportation in their call center,
via the web, or by email;
• assigning approvable trips based first upon the medically appropriate mode of
transportation, then by enrollee’s choice among participating transportation vendors, and
finally, at the discretion of the transportation broker.
• generating prior authorizations according to the parameters established by the NYSDOH;
• accepting, investigating and resolving complaints from Medicaid enrollees, medical
providers and transportation vendors;
• developing grouped rides to common medical destinations;
• referring identified potential abuse and proposing potential cost savings initiatives to
NYSDOH; and
• performing quality assurance surveys.
All participating transportation vendors should obtain access to the transportation broker’s web-
based systems to attest, cancel or request changes to trips, etc.
Transportation vendors, enrollees and medical providers in should consult MAS by visiting
their website: https://www.medanswering.com/.
Inappropriate Prior Authorization Practices
Generally, prior authorization must be obtained before transportation expenses are incurred.
Prior authorization is not required for emergency ambulance transportation or Medicare-
approved transportation by an ambulance service provided to an MA-eligible person who is also
eligible for Medicare Part B payments. If transportation services are provided in accordance with
section 505.10(e)(7), the individualized education program or interim or final individualized
family services plan of an MA eligible person will qualify as the prior authorization required by
this subdivision. Requests for prior authorization may be made by the MA enrollee, his or her
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 15 of 52
representative, or an ordering practitioner. The enrollee, his or her representative, or ordering
practitioner must make the request in the manner required by the prior authorization official.
Each social services district must inform applicants for and enrollees of MA of the need for prior
authorization in order for transportation expenses to be paid under the MA program and of the
procedures for obtaining such prior authorization. The prior authorization official may approve or
deny a request for prior authorization or require the ordering practitioner to submit additional
information before the request is approved or denied.
It is inappropriate for a transportation provider (TP) to request prior authorization from the
Prior Authorization Official.
Requests for Prior Authorization
Generally, all trips must be prior approved before the trip takes place. The Medicaid program
requires all Medicaid providers to submit a claim for payment for a completed trip within ninety
(90) days of the date of service unless submission of the claim is outside the control of the
provider. Since the prior authorization process is an inherent step in the claiming process, it is
also governed by the 90-day claiming regulation at
18 NYCRR §540.6.
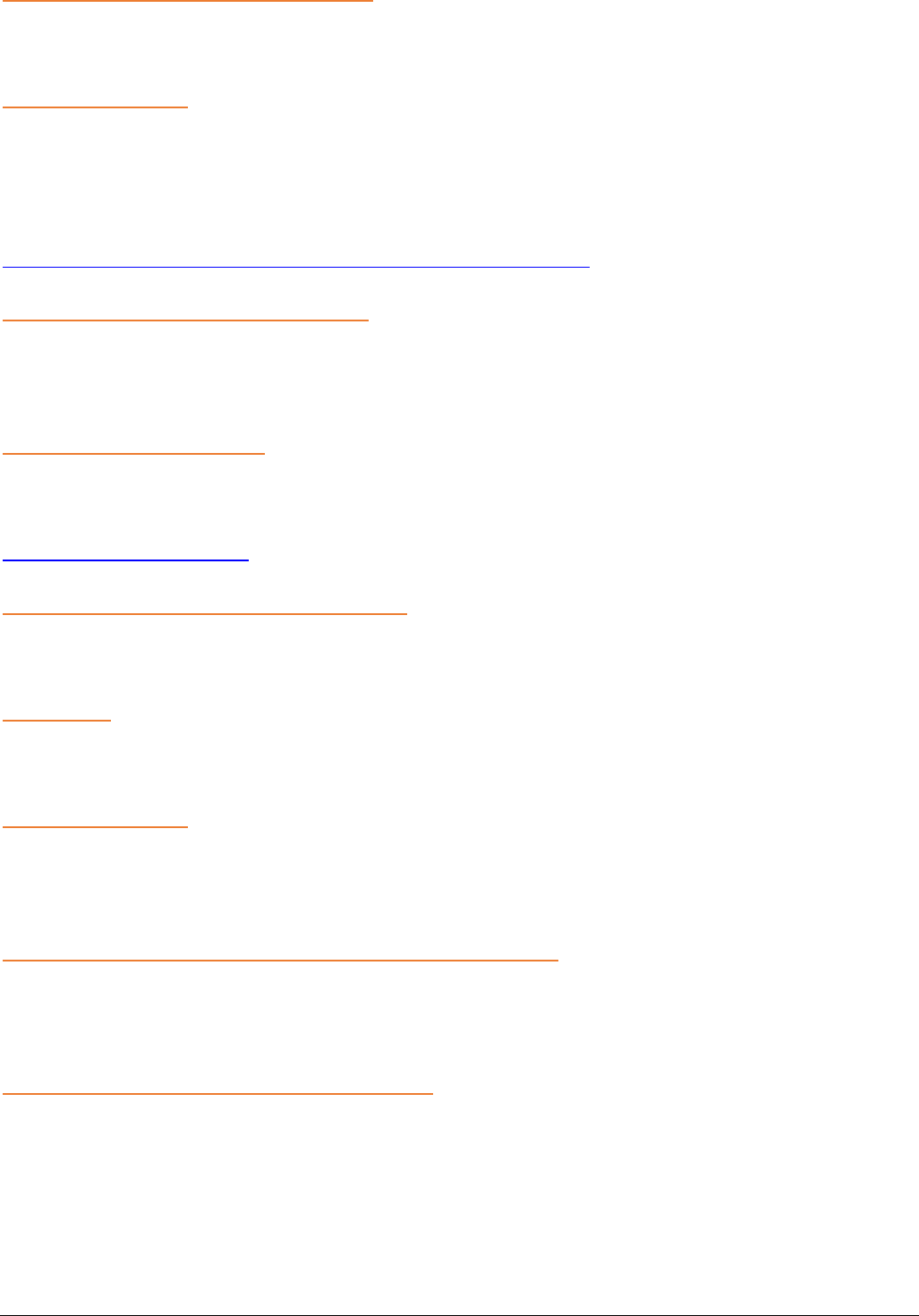
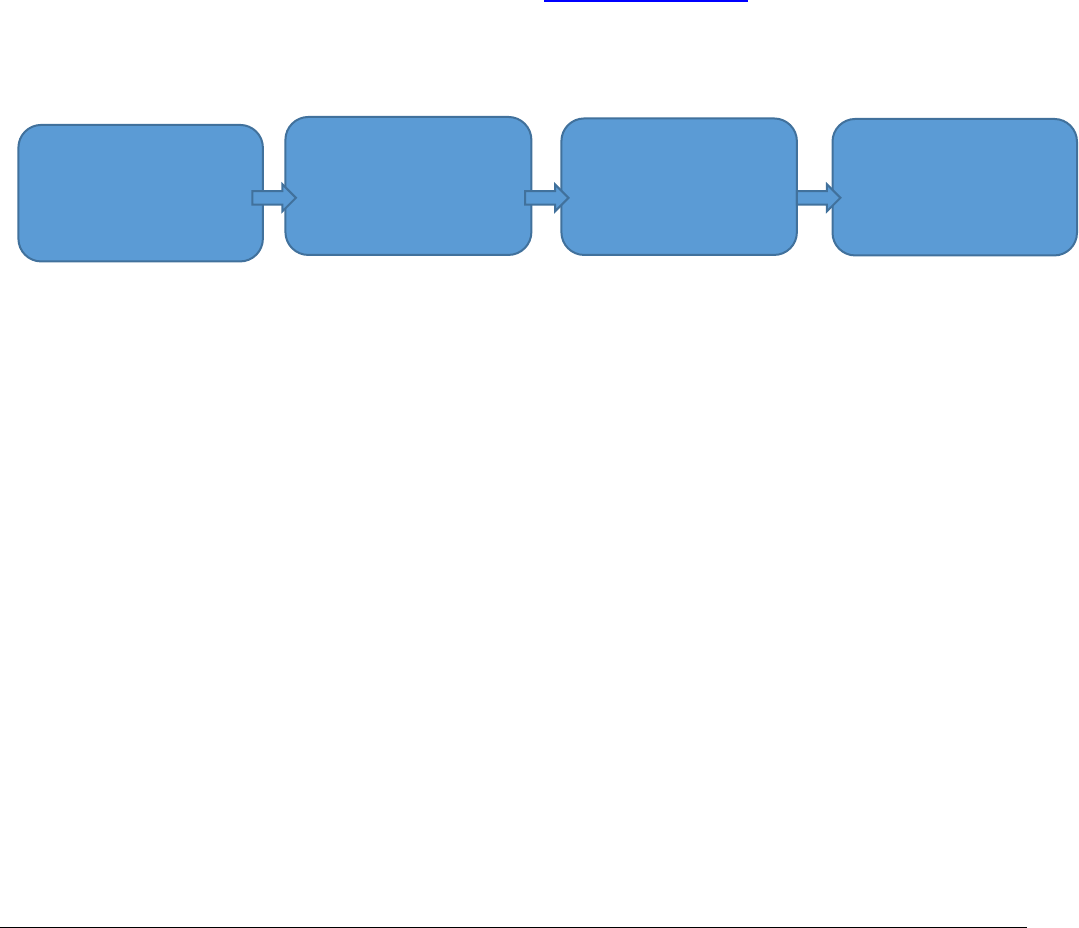
Please see the diagram below on the process of obtaining a Prior Authorization (PA) number
which is required to submit a claim for payment.
Many requests for prior authorization submitted greater than 90 days after the date of service
are done so because transportation providers cannot confirm an enrollee’s Medicaid eligibility
as the eligibility determination is pending action by the local department of social services or
other eligibility gateway. In these instances, the Medicaid program considers the request and
claim submission to be outside the transportation provider’s control. Consequently, the
Medicaid program expects transportation providers to diligently monitor the eligibility
verification system to determine when Medicaid eligibility is retroactively approved, and
the date for which eligibility is effective.
All trip attestations should be sought within thirty (30) days of the date of service.
Requests submitted beyond this time are subject to payment disallowance.
• If the enrollee does not become Medicaid eligible for transportation services on the date of
service, the request for prior authorization will be denied.
PA Official sends trip
to TP
TP performs trip and
attests trip completion
to PA Official
TM receives a Prior
Authorization (PA)
number from
eMedNY
PA Official sends PA
info to TP, TP bills
eMedNY

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 16 of 52
• For enrollees with effective retroactive eligibility, a transportation provider may submit a trip
attestation up to 120 days from the date eligibility is established on the eligibility verification
system.
• Requests submitted beyond this 120-day period will be denied.
All modifications/corrections must be requested prior to attestation (within 30 days of eligibility
verification). For requests involving changes/corrections to existing prior authorizations, the
following applies:
• If the request is submitted within 90 days of the date of service, the Department (or
Department’s prior authorization official) may approve the request to change the existing
prior authorization.
• If the request is more than 90 days from the date of service but less than 30 days from the
date the prior authorization was issued, the Department (or the Department’s prior
authorization official) may approve the request to change the existing prior authorization.
• If the request was more than 90 days from the date of service, and more than 30 days
have passed since the date that the prior authorization was originally issued, the
Department (or the Department’s prior authorization official) may deny the request for a
change in the authorization.
For requests involving third party insurance denials (which pertain primarily to ambulance
providers):
• All requests will require a written copy of the denial
• If the request is submitted within 90 days of the date of service, the Department (or
Department’s prior authorization official) may approve the request to issue a prior
authorization.
• If the request is more than 90 days from the date of service but less than 30 days from
the date of the remittance statement from the third-party insurance company denying
payment, the Department (or Department’s prior authorization official) may approve the
request to change the existing prior authorization.
• If the request was more than 90 days from the date of service, and more than 30 days
have passed since the date of the remittance statement from the third-party insurance
company denying payment, the Department (or Department’s prior authorization official)
may deny the request for a change in the authorization.
Requests dated more than 90 days beyond the service date must be sent to the Department of
Health via either of the following methods:
eFax: (518) 486-2495

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 17 of 52
Non-Emergency Transportation of Restricted Enrollees
The Department may restrict an enrollee’s access to Medicaid covered care and services if,
upon review, it is found that the enrollee has received duplicative, excessive, contraindicated or
conflicting health care services, drugs or supplies (18 NYCRR §360-6.4).
The State medical review team designated by the Department performs Medicaid enrollee
utilization reviews and identifies candidates for the Restriction Program. In these cases, the
Department may require that the enrollee access specific types of medical care and services
through a designated primary provider or providers.
The primary provider is a health care provider enrolled in the Medicaid program who has agreed
to oversee the health care needs of the restricted enrollee. The primary provider will provide
and/or direct all medically necessary care and services for which the enrollee is eligible within the
provider’s category of service or expertise. Primary providers include:
• Physicians
• Clinics
• Inpatient Hospitals
• Pharmacies
• Podiatrist
• DME Dealers
• Dentists
• Dental Clinics
When a Medicaid enrollee has been restricted to a primary provider, only the primary
provider is allowed to order transportation services for the enrollee. This applies to all
modes of non-emergency transportation and includes cases where the enrollee’s primary
physician or clinic has referred the enrollee to another provider. In such situations, requesting
transportation remains the responsibility of the primary provider. Transportation providers
should use the identification number of the primary provider when obtaining eligibility
information and submitting claims.
2.4 Transportation Provider Requirements and Responsibilities
To participate in the New York State Medicaid program, a provider must meet all applicable
Federal, State, County and Municipal requirements for legal operation. In addition to the policies
set forth in this Manual, and in other directives related to Medicaid policy, the Medicaid program
expects the following of all providers:
• All drivers, during their employment, must be at least eighteen (18) years of age and have
a current, valid driver’s license from New York or another state to operate the transportation

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 18 of 52
vehicle to which they are assigned.
• All drivers and escorts will be courteous, patient, and helpful to all passengers and be neat
and clean in appearance.
• Driver or escorts must not use alcohol, narcotics, illegal drugs or drugs that impair ability
to perform while on duty and no driver shall abuse alcohol or drugs at any time.
• At no time will drivers or escorts smoke while in the vehicle, while involved in enrollee
assistance, or in the presence of any enrollee.
• Drivers and escorts shall provide necessary assistance, support, and oral directions to
passengers.
• Transportation providers can only provide transportation services that have been
authorized by the prior authorization official(s).
• Transportation providers shall wait at least fifteen (15) minutes after the scheduled pick-up
time before “no-showing” the enrollee at the pick-up location. The network provider shall
document all “no shows.”
• Rides in duration of less than one (1) hour (barring exceptions based on location or acute
circumstances such as inclement weather and unexpected traffic situations).
• All vehicles must be registered with the NYS Department of Motor Vehicles, in the
appropriate registration class, and be properly insured.
• Have two-way radio or cellular phone communication capability.
• Provide valid DMV registration with expiration date and valid insurance ID card with
expiration date.
• Be equipped with properly functioning air conditioner/heater/defrosters.
• Each vehicle shall have the ability to properly secure child safety seats, when provided by
an enrollee or caregiver.
• Be equipped with a properly functioning speedometer and odometer.
• Have a clean interior and exterior.
• Have a smoking prohibition use notice posted in all vehicle interiors, easily visible to the
passengers.
• Include a vehicle information packet containing vehicle registration, insurance card, and
accident procedures and forms. The accident procedure will include a requirement that the
transportation provider informs the Transportation Broker of all accidents and incidents
within 48 hours.
• Be sufficiently stocked with personal protective equipment for drivers in accordance with
OSHA Standards 1910.1030 and 1910.134, and any other applicable statute or
regulation.
• All vehicles are equipped with GPS capability and transmit coordinates and other related
data to the broker as required.
• Follow all Cleaning/Disinfection requirements and reporting as outlined by the
Department.
• Passengers must have their seat belts buckled while they are inside the vehicle. The driver
shall assist passengers who are unable to fasten their own seat belts if requested.
• The driver shall not put the vehicle in motion until all passengers have been properly
secured.
• The number of persons in the vehicle, including the driver, shall not exceed the vehicle
manufacturer’s approved seating capacity.
• Upon arrival at the destination, the vehicle shall be parked or stopped so that passengers
do not have to cross streets to reach the entrance of their destination.
• If passenger behavior or other conditions impede the safe operation of the vehicle, the
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 19 of 52
driver shall park the vehicle in a safe location out of traffic and notify their dispatcher or 911
to request assistance.
Providers of all levels of medical transportation will encounter patients/passengers who may
have infectious diseases. To protect the health and well-being of everyone, all providers must
follow CDC Standard Precautions for All Patient Care -
https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html
Transportation providers cannot refuse to pick up a Medicaid member based on their medical
condition or status. Any pattern of transport denial linked to an enrollee’s physical appearance,
disability, and other protected classes is strictly prohibited. 42 USC 12182: Prohibition of
discrimination by public accommodations
Additionally, as employers, all transportation providers must abide by OSHA Standards
1910.1030 (Bloodborne Pathogens), 1910.134 (Respiratory Protection), as well as OSHA’s
“General Duty Clause”.
https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.1030
https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134
Transportation Provider Network Credentialing
For purposes of credentialing, transportation providers must provide to the Transportation
Broker or the Department:
• Valid New York or other valid state driver license.
• Valid vehicle registration.
• Valid vehicle inspection.
• Valid Certificate of Insurance.
• Valid insurance identification cards.
• Confirmation of enrollment as a Medicaid transportation provider.
Medicaid Enrollment Does Not Supplant Local Regulations
Title 18 NYCRR §505.10(e)(6) indicates that providers must, regardless of Medicaid enrollment
status, comply with applicable regulatory requirements. For ambulette, taxi and livery
companies, this may include local licensure by a municipality or a Taxi and Limousine
Commission.
Failure to comply with local regulations may result in termination from Medicaid enrollment, as
well as action by the local regulatory entity.
Source: November 2009 Medicaid Update
Vehicle Ownership or Leasing the Insurance for Categories of Service 0601, 0602, and 0603
Medicaid program transportation service providers for category of service 0601 (Ambulance),
0602 (Ambulette), and 0603 (Taxi) are personally and directly responsible for their fleet of
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 20 of 52
vehicles. These category of service providers must own the vehicles outright or be personally
responsible for the vehicles pursuant to a vehicle lease agreement. The provider may enter into
a lease agreement with a motor vehicle manufacturer or with a licensed vehicle dealership.
Vehicle leases are acceptable as long as the lease agreement is in the name of the Medicaid-
enrolled transportation service provider and the vehicle is registered to the Medicaid-enrolled
transportation service provider.
Further, vehicles must be insured and maintained by the Medicaid-enrolled transportation service
provider.
It is unacceptable for a Medicaid-enrolled transportation service provider to enter into any
arrangement whereby the provider uses, or leases vehicles registered to, insured and/or
maintained by another individual or entity. Such an arrangement has the potential of bypassing
significant safety and financial controls that are fundamental to the integrity of the Medicaid
program and the safety of the Medicaid enrollees.
Providers in violation of this policy must continue to meet these standards concerning vehicle
ownership, registration, maintenance, and insurance. Those providers deemed in violation of this
policy are subject to penalty, including disenrollment from the Medicaid program. Note: New
transportation provider applicants must adhere to these requirements at the time of application.
Source: December 2015 Medicaid Update
Vehicle Ownership for Exemption for Categories of Service 0605 and 0609
Medicaid transportation providers enrolled in categories of service 0605 Livery/Black Car (NYC
Only) or 0609 Transportation Network Company/High Volume For-Hire-
Service are exempt from the requirements listed in the section above “Vehicle Ownership or
Leasing the Insurance for Categories of Service 0601, 0602, and 0603”. Under these two
categories of service, providers may employ drivers who own and operate their own vehicles.
Please note, Medicaid transportation providers that are enrolled in these categories of service
must comply with all local municipal requirements, including being licensed by the applicable
Taxi and Limousine Commission governing the service area, and with all requirements of the
NYS Department of Motor Vehicles.
Source: December 2018 Medicaid Update
Subcontracting Transports
Medicaid program transportation service providers are personally and directly responsible for
transporting Medicaid enrollees. These responsibilities may not be assigned, delegated or
subcontracted out. Such an arrangement has the potential of bypassing significant safety and
financial controls that are fundamental to the integrity of the Medicaid program and the safety of
Medicaid enrollees.
Due to mechanical breakdowns and other acute circumstances, transportation providers may
face times when the number of available vehicles registered to the provider does not meet the
need for services. Formerly, the Medicaid program allowed on a short-term basis Medicaid-
enrolled Provider A to subcontract with or lease vehicles from Medicaid-enrolled Provider B or

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 21 of 52
other entity in order to ensure the provision of services to the enrollee. The Medicaid program
no longer allows these arrangements.
If a Medicaid transportation provider encounters a circumstance when his supply of provider-
registered vehicles does not meet the need for services, the provider must alert the appropriate
transportation broker as soon as possible so that the transportation broker may find an available
provider to perform the necessary trip or trips. Please be reminded that Medicaid transportation
brokers are accessible 24/7 by telephone and can be identified using the contact list available
online at http://www.emedny.org/ProviderManuals/Transportation/index.html.
Source: December 2015 Medicaid Update
Updated Requirements for Volunteer Driver Organizations
The New York State Department of Health recognizes that volunteer drivers are a valuable
component of the Medicaid Transportation Program, especially in transporting enrollees to
necessary medical services in rural areas.
All volunteer driver organizations must be enrolled as Medicaid providers and can only
assign trips to volunteer drivers who are affiliated with their organization.
Volunteer driver organizations are required to:
• Perform criminal background checks and driver's license verifications before assigning
any Medicaid funded trips to a volunteer driver; and
• Ensure that all drivers maintain the appropriate vehicle liability insurance.
Volunteer drivers must:
• Maintain a valid license that is appropriate for the size and type of vehicle they are
operating;
• Provide curb to curb transportation;
• Maintain all required records necessary to support a Medicaid transportation claim;
• Meet or exceed Medicaid quality standards (e.g., no smoking, vehicle cleanliness, etc.);
and
• Maintain at least the minimum insurance requirements in accordance with the New York
State Department of Motor Vehicles.
Source: March 2016 Medicaid Update
Vehicles used by volunteer drivers must follow all requirements outlined in section 2.4.
2.5 Record Keeping Requirements and Reporting
In accordance with Title 18 NYCRR §504.3(a) and 517.3(b), transportation providers will be
reimbursed only when contemporaneous, complete, acceptable, verifiable records are available
upon request to the State in connection with an audit, investigation or inquiry. The documentation
below is required for every leg of a trip and must be maintained for a period of six (6) years
following the date of payment. If any of the required information is incomplete, or deemed
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 22 of 52
unacceptable or false, any relevant paid reimbursement will be recouped, and the provider may
be subject to other statutory or regulatory liability, financial damages and sanctions.
Attestation and Claim Detail (Applicable to All Providers Except Ambulance)
Effective March 1, 2016, in addition to historically required acceptable trip verification, the
Department requires the full printed name and signature of the driver providing the transport
attesting that the referenced trip was completed. The full list of required trip verification
information now includes, at a minimum:
• The Medicaid enrollee’s name and Medicaid identification number;
• The date of the transport;
• Both the origination of the trip and time of pickup;
• Both the destination of the trip and time of drop off;
• The vehicle license plate number;
• The driver’s license number;
• The full printed name and signature of the driver providing the transport; and
• An attestation from the driver that the trip was completed. (Indication of no show if trip did
not take place).
Electronic Records
The Department will allow transportation providers to comply with these record keeping
requirements by: (1) substituting the written signature of the driver providing the transport
with a unique identifying electronic signature, and (2) requiring drivers attest that the trip
has been completed by using an electronic verification transmission that records both
the trip drop-off and pick-up destination coordinates.
Therefore, the driver "clicking" to confirm trip completion verification at the end of each ride can
be used as long as it satisfies the Department's requirement for a "contemporaneous, complete,
acceptable, verifiable" record that the driver has both provided the trip and attested to its
completion to support Medicaid claims - and that the transportation provider can produce this
documentation with an accurate, system-generated, unmodifiable date and time stamp for each
leg of a billable trip, including the pickup and drop-off, for the required six-year period.
The use of the electronic signature option does not exempt transportation providers from any of
the current record keeping requirements or prospective audit of such record keeping by
enforcement agencies.
Source: January 2019 Medicaid Update
Supplemental Documentation
The following items presented as the only evidence of a trip are not considered acceptable
documentation. However, these documents may be considered supplemental to additional
required documentation and can be presented to supplement required documentation:

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 23 of 52
• A driver/vehicle manifest or dispatch sheet;
• Issuance of a prior authorization by an approved official with subsequent checkmarks;
• A prior authorization roster; or
• An attendance log from a day program.
Reminder – Requirements under 505.10 Transportation for Medical Care and Services
Providers must comply with 18 NYCRR § 505.10 in its entirety.
https://regs.health.ny.gov/volume-c-title-18/content/section-50510-transportation-medical-care-
and-services
Source: December 2015 Medicaid Update
Accident/Incident Reporting
An “accident” is defined as a vehicle colliding with another vehicle, a physical structure, an
object, a person, or an animal.
An “incident” is defined as an occurrence, breakdown, or public disturbance that interrupts the
trip causing the driver to stop the vehicle, such as when a passenger or driver becomes unruly
or ill.
All New York State (NYS) Medicaid-enrolled transportation providers must follow expanded
accident/incident reporting protocol. Effective January 1, 2022, all events must be reported
using the NYSDOH NEMT Accident and Incident Report.
All providers should report these events to the prior authorization official and/or Department, in
accordance with the 10 NYCRR Part 800.21:
(q) upon discovery by or report to the governing authority of the ambulance service, report
to the Department’s Area Office by telephone no later than the following business day and
in writing within 5 working days every instance in which:
(1) a patient dies, is injured or otherwise harmed due to actions of commission or
omission by a member of the ambulance service;
(2) an EMS response vehicle operated by the service is involved in a motor vehicle
crash in which a patient, member of the crew or other person is killed or injured to the
extent requiring hospitalization or care by a physician;
(3) any member of the ambulance service is killed or injured to the extent requiring
hospitalization or care by a physician while on duty;
(4) patient care equipment fails while in use, causing patient harm;
(5) it is alleged that any member of the ambulance service has responded to an
incident or treated a patient while under the influence of alcohol or drugs while on
duty.
(r) on or in a form approved by the department, maintain a record of all unexpected,
authorized EMS response vehicle and patient care equipment failures that could have
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 24 of 52
resulted in harm to a patient and the corrective actions taken. A copy of this record shall
be submitted to the department with the EMS service’s biennial recertification application.
Ambulance providers may submit the Bureau of Emergency Medical Services
(BEMS) Reportable Incident Form (DOH-4461) in place of the NYSDOH NEMT Accident and
Incident Report. Transportation providers must submit the forms to their transportation brokers
within 48 hours of the events. The NEMT Accident and Incident Report and additional detail on
reporting requirements are found on the transportation brokers websites.
Source: November 2021 Medicaid Update
GPS Compliance Requirement
Effective April 3, 2023, New York State NYSDOH requires all Transportation Providers (TP) to
be fully Global Positioning System (GPS) compliant.
1
For a trip to be considered fully GPS-
compliant, the Transportation Provider will submit the starting point, end point, and all GPS
coordinates along the trip (“breadcrumb data”) to the Transportation Broker. Transportation
Providers must take necessary steps to ensure GPS compliance.
The use of GPS data will be used to increase program integrity, ensure enrollee safety, aid in
the development of future policies, and assist in the reduction of fraud, waste, and abuse.
For Transportation Providers currently using a Third-Party Intermediary (TPI) / Advanced
Transportation Management Systems (ATMS) billing or routing software:
• Make sure all drivers have GPS capability and that each trip’s GPS data is being
accurately routed.
• For a complete list of TPIs/ATMS that are compliant with the appropriate brokers software
or to ensure that your TPI/ATM is compliant please contact the transportation broker.
Loss of Records Due to Unforeseen Incident
Federal law and State regulations require Medicaid providers to maintain financial and health
records necessary to fully disclose the extent of services, care, and supplies provided to
Medicaid enrollees. This is stated in Title 18 of the New York Code of Rules and Regulations at
§504.3:
By enrolling, a provider agrees:
To prepare and maintain contemporaneous records demonstrating its right to receive payment
under the Medicaid program and to keep for a period of six years from the date the care,
services or supplies were furnished, all records necessary to disclose the nature and extent of
services furnished and all information regarding claims for payment submitted by, or on behalf
of, the provider and to furnish such records and information, upon request.
Additional record keeping requirements for transportation providers can be found in the previous
section of this Manual.
1
GPS compliance is required unless special exemption is granted by the NYS Department of Health
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 25 of 52
Transportation providers whose paper and/or electronic records are damaged by fire, flood or
other disaster are required to notify the New York State Office of the Medicaid Inspector General
(OMIG) of the loss of their records. This self-reporting notification must include specific details of
the event causing the loss of records, type of required records lost, date/s of service impacted by
the loss, and documents/photographs substantiating the loss. Information on self- reporting can
be found online at https://omig.ny.gov/submission-checklist-and-faqs.
Additionally, providers must notify any other State or local regulatory agency of its loss as
required by those regulatory agencies, including a Taxi and Limousine Commission (taxi, livery,
and ambulette providers), or the New York State Department of Health (ambulance providers),
and/or the New York State Department of Motor Vehicles (ambulette providers).
Source: September 2016 Medicaid Update
2.6 Complaints and Complaint Reporting
Transportation Broker Complaints
Medicaid enrollees or their representatives and/or medical providers or their representatives
and/or transportation providers may file complaints against transportation brokers to the
Department. The Department will review all complaints and investigate credible complaints as
appropriate. Confidentiality of complainant-identifying information is maintained to the
extent practicable.
Complaints are received by the NYSDOH via the following methods:
Telephone: (518) 473-2160
Email: MedTrans@health.ny.gov
Service Complaints
Medicaid enrollees or their representatives, and/or medical practitioners or their representatives,
may file complaints against transportation providers when it is believed that safe and quality
transportation services were not provided to a Medicaid enrollee.
Information regarding the nature of complaints received regarding the services provided by
entities transporting Medicaid enrollees is forwarded to the transportation provider or entity
regarding whom the complaint was lodged, and/or the county department of social services
(DSS), and/or the State’s contracted transportation broker, and, where applicable, the Office of
the Medicaid Inspector General and/or other enforcement agencies. Confidentiality of
complainant-identifying information is strictly maintained.
Service Complaints can be directed to MAS at: https://www.medanswering.com/comments-or-
concerns/ or to the NYSDOH. Service complaints received by NYSDOH will be routed to MAS.
2.7 Claims and Reimbursement
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 26 of 52
Reimbursement Fees
The current Medicaid transportation fee schedule is located online at:
https://www.emedny.org/ProviderManuals/Transportation/index.aspx
The transportation broker is responsible for negotiating reimbursement directly with network
transportation providers. The negotiated rates will supersede the current fee schedule.
It is illegal for any transportation provider to pay, or even offer to pay a Medicaid
enrollee, in exchange for using its services. In this context, pay means provide or offer
to provide anything of value, including but not limited to money, drugs, free or
discounted personal transportation or housing.
Medicaid members shall never pay a copay for NEMT, and drivers and transportation
providers shall never request payment directly from a member.
Multiple Dates of Service
For each date of service, a provider transports an enrollee; a separate claim line must be
submitted. For example, Mrs. Jones was transported round trip on July 1, 2 and 3. Three
separate claim lines should reflect two units on each of date of service.
Note: Claim edit code definitions are listed on the last page/s of a remittance statement.
Additionally, claim edit 7–0 - PA UNITS OR PAYMENT AMOUNT EXCEED–D - will deny
claims which contain more daily units than allowed by a prior authorization.
Source: July 2009 Medicaid Update
Contracted Billing Agents
Due to the complexities involved with billing insurance companies for services rendered, many
transportation vendors use a private billing agent to submit claims to the Medicaid program on
their behalf.
Transportation vendors should note that they, not their contracted billing agent, are ultimately
responsible for any inappropriate billing identified post-payment which is attributed to their
company. Therefore, it is imperative that transportation vendors, in addition to their billing
agents, be aware of and compliant with all applicable Medicaid policies.
Additionally, billing agents must enroll as a “Service Bureau” with the New York State Medicaid
program. Even if the billing agent is enrolled as a Medicaid service vendor, they must separately
enroll as a Service Bureau in order to submit claims on behalf of another vendor.
Source: February 2010 Medicaid Update
Enhanced Mileage Accuracy
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 27 of 52
Transportation providers historically have submitted mileage claims that round the fractional
mileage distance from the nearest tenth of a mile traveled to the next highest whole number
(e.g., from 2.7 miles to 3.0 miles). The New York State Department of Health (the Department)
has determined that the current capabilities of the prior authorization and claims payment
systems can accommodate fractional mileage claims that reflect distance to the nearest tenth of
a mile. The submission of fractional mileage claims enhances payment accuracy, reduces
Medicaid overpayments, achieves alignment with current Medicare mileage reimbursement
policy, and better reflects the advent of geocoded trip recording technologies.
Effective for dates of service on or after August 1, 2019, claims for loaded mileage must be
reported as fractional units to the tenth of a mile (for trips totaling less than one mile, enter
a “0” before the decimal point (e.g. 0.9). Rounding mileage units up to the nearest whole
number is not allowed for claims with dates of service on or after August 1, 2019. Rounded-up
claims may be deemed fraudulent and therefore subject to any recoveries and associated
penalties by enforcement agencies. Transportation providers who are unable to comply with
the August 1, 2019 fractional mileage reporting requirement, due to software limitations or other
reasons, may round mileage units down to the nearest lowest whole number until a time
determined by the Department.
As always, the Medicaid program will only reimburse transportation providers for “loaded” miles.
Loaded miles are those miles during which an enrollee occupies the vehicle.
Source: May 2019 Medicaid Update
Rides Grouped by the Transportation Provider
All ambulette, taxi, or van providers who transport more than one Medicaid enrollee at the same
time in the same vehicle and who are reimbursed for passenger-laden mileage should claim
only for the actual number of miles from the first pick-up of an enrollee to the final destination
and drop-off of the last Medicaid passenger.
For example, Ace Company’s reimbursement has been established at $20.00 per one- way
pick-up fee plus $1.00 per loaded mile. Ace is authorized to transport Mrs. Jones to her
Friday morning clinic appointment, a one-way mileage of thirteen (13) miles; and Mr. Frank
to the same clinic at the same time, a one-way mileage of seven (7) miles.
Ace will pick up both enrollees in the same vehicle as they live along the same route. Ace
should claim the base fee and mileage fee of 13 miles for Mrs. Jones, as she was the first
passenger to be picked up. Ace should only claim the base fee for Mr. Frank. The 7 miles
authorized for Mr. Frank duplicate the concurrent mileage paid under Mrs. Jones’ claims.
Ace should not claim these 7 miles.
If a provider is reimbursed on a one-way pickup (i.e., flat) fee only (no mileage reimbursement),
regardless of the number of miles transported, then this policy does not apply.

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 28 of 52
For Medicaid enrollees who reside outside their county of eligibility, the rule for ordering mileage
reimbursement is the same as that which applies to all other Medicaid enrollees of the
residential county.
Preferred Provider Opportunities (PPO)
Preferred Provider Opportunities (PPO) are designed to promote collaboration between medical
and transportation providers to improve communication and operational practices that result in
better access to healthcare for Medicaid enrollees.
Once established, PPOs are monitored by the NYSDOH to ensure Medicaid enrollees’ access
to healthcare is being achieved. Regular stakeholder meetings are mandatory to ensure
challenges and concerns of all parties are addressed. Furthermore, quality assurance and
Medicaid enrollee satisfaction are measured regularly to determine the program’s success in
meeting its goals.
Expectations:
• No PPO Trip Invoice can be refused or reassigned.
• Maintain compliance with all NYSDOH Medicaid NEMT Policies and Procedures (i.e., all
vehicles are required to provide GPS data for all transports).
• On time performance for picking up enrollees - within 15 minutes of scheduled pick-up
time.
• On time performance for hospital discharges. TP must be at Hospital within 60 minutes of
Trip Invoice Assignment.
• NYSDOH, Medicaid Provider, and Transportation Providers are required to attend
stakeholder meetings regularly.
• Excellent, frequent, and appropriate communication between the TP and Medical provider
is expected and required.
Multiple Riders from the Same Location
Medicaid does not pay for transportation of cohabitants needing transportation to the same
destination, even if each cohabitant has a medical appointment. For example, a mother and her
son live at 1 Cherry Tree Lane, and both have appointments at 7 Murray Avenue on November
1st. In this circumstance, the Medicaid program will authorize one trip, and indicate there will be
an additional rider. The transportation vendor will not be authorized a separate compensable trip
for the additional rider.
Typically, cohabitants that fall under this category are those related by marriage or birth, but
may include roommates, friends, etc. who are residing, temporarily or otherwise, at the address.
This policy does not apply to persons residing in apartment complexes where each person lives
in a separate apartment, nor does it apply to adult homes, nursing facilities, etc.
Toll Reimbursement

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 29 of 52
The Medicaid program will reimburse only for the actual costs incurred by a transportation
provider while transporting a Medicaid enrollee. When tolls are incurred, the toll is assessed per
vehicle, not per rider, and should be billed according to the actual toll charged. Therefore, if a
vehicle is transporting more than one rider on the same trip, the provider may bill one
unit per charged crossing, not one unit per passenger.
E-Z Pass Customers
E-Z Pass customers, should bill Medicaid for the actual toll amount charged to their E-Z Pass
account while transporting a Medicaid enrollee or enrollees. Non E-Z Pass customers who pay
tolls by mail, will only be reimbursed at the current E-Z Pass rate. Current toll rates can be found
here: Toll Rates | New York State Bridge Authority (ny.gov)
Providers may enroll in the E-Z Pass program online at http://www.e-zpassny.com.
Congestion Surcharge Pricing and Reimbursement Affecting Medicaid Transportation Providers
The enacted 2018-19 State Budget (S.7509-C / A.9509-C) contained statutory provisions to
reduce traffic in a "congestion zone" in the New York City Borough of Manhattan, south of
and excluding
6th Street. Effective January 1, 2019, for-hire transportation for a single
passenger that originates, terminates, or enters the congestion zone from anywhere in the State
must pay a surcharge of $2.75 per trip. Pool vehicles that transport two or more passengers
with separately requested transportation will be surcharged $0.75 per passenger.
Accordingly, this surcharge will be applied to Medicaid transportation providers conducting
multi-loaded or group rides. This surcharge will be applied to Medicaid taxi / livery, green car,
black car, and ridesharing / transportation network vehicles (ambulance and ambulette vehicles
are exempt from the surcharge).
Registration and Fee:
Medicaid transportation providers, like other transporters subject to the surcharge, must file an
application for a Certificate of Registration in a manner prescribed by the Commissioner of
Taxation and Finance. A registration fee of $1.50 must accompany the application. However,
transportation providers who will be subject to the surcharge no more than one time in any
single calendar month are not required to register. Registration is valid for three years and then
subject to renewal upon payment of the registration fee. The Certificate of Registration will
indicate the transportation provider's vehicle or vehicles and is not assignable or transferrable
to other companies.
Paying the Surcharge:
Medicaid transportation providers, like other transporters subject to the surcharge, must file a
monthly return with the Commissioner of Taxation and Finance within 20 days after the end of
each month that indicates the number of trips and pool passengers. The form of the return,
which can be electronic, will be prescribed by the Commissioner. At the time of filing the return,
transportation providers must pay the amount of all surcharges to the Commissioner. Failure to
pay the surcharge when due will result in a 200 percent surcharge amount penalty.
Transportation providers must not ask Medicaid enrollees to pay the surcharge.

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 30 of 52
Reimbursement for Fee-for-Service Transportation Providers:
Transportation providers will be reimbursed for the cost of the surcharge through the Medicaid
Fee-for-Service (FFS) billing system. Medicaid Transportation providers will use the A0170
Procedure Code for tolls with the ”TU" modifier for a single trip ($2.75) and the ”TK"
modifier for pool trips ($0.75 per person).
Reimbursement for Managed Long Term Care Transportation Providers:
Managed Long Term Care plans receive a regional adjustment to the capitated rate.
Transportation providers receive payment in accordance with the terms of the contract with the
Managed Long Term Care plan.
Record Keeping:
Transportation providers subject to the surcharge must keep records of every trip provided or
arranged and amounts paid in a form required by the Commissioner of Taxation and Finance.
Source: November 2018 Medicaid Update
Situations Where Medicaid Will Not Provide Reimbursement and/or May Seek Post-Payment Recoupment
Reimbursement is not provided for any mode of transportation when any of the following
situations exists:
• The individual is not eligible for Medicaid on the date of service;
• Prior authorization for the non-emergency transport was not obtained;
• The claim is not submitted to the Medicaid program within the required timeframe in the
required format with required information;
• The medical service to which the transportation occurred is not covered by the Medicaid
program (i.e., Medicaid will only consider payment of transportation services to and from
care and services covered by the Medicaid program);
• The transportation service is available to others in the community without charge;
• The Medicaid enrollee is restricted to a primary provider, and the claim identifies another
ordering provider’s identifying information;
• There is a fee listed but effort is never made to collect the fee from individuals who are not
enrolled in the Medicaid program;
• The provider is out of compliance with applicable licensure requirements;
• The service is provided by a medical institution or program and the cost is included in that
institution’s or program’s Medicaid fee; or
• Transportation services are not actually provided to a Medicaid enrollee.
Reporting of Vehicle and Drive License Numbers
On claims for which an ambulette vehicle was used, providers are required to include both:
• The driver license number of the individual driving the vehicle; and
• The license plate number of the vehicle used to transport the enrollee.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 31 of 52
If a different driver and/or vehicle returns the enrollee from the medical appointment, the license
number of the driver and vehicle used for the origination of the trip should be reported on the
claim.
Source: November 2005 Medicaid Update
The Department has reached agreement with the Office of the Medicaid Inspector General and
the Attorney General’s Medicaid Fraud Control Unit to require that claims submitted by
taxi/livery providers include both the driver license and vehicle license plate number. The
Department agrees that reporting this information will aid in its intent to ensure quality services
and program integrity.
Effective May 24, 2018, claims that do not include the required fields will be denied for edit
00267, “VEHICLE LICENSE PLATE / DRI’ER'S LICENSE NUMBER REQUIRED.”
Sources: December 2015 Medicaid Update; April 2018 Medicaid Update
Ambulance Services – Use of Claim Modifier
All ambulance providers are required to include the appropriate base fee procedure code
(HCPCS Code), and mileage code (when applicable), on submitted ambulance (category of
service 0601) claims. Ambulance providers must also include an origin/destination modifier in each
claim submission
The origin/destination modifier is not required on the Prior Authorization generated for the
service.
Similar to Medicare, for each base line item, the trip origin is reported by using a modifier in the
first position and the destination is reported using a modifier in the second, as follows:
D
=
Diagnostic or therapeutic site other than P or H when these are used as
origin codes
E
=
Residential, domiciliary, custodial facility (other than 1819 facility)
G
=
Hospital-based End-Stage Renal Disease (ESRD) facility
H
=
Hospital
I
=
Site of transfer (e.g. airport or helicopter pad) between modes of
ambulance transport
J
=
Freestanding ESRD facility
N
=
Skilled nursing facility
P
=
Physician's office
R
=
Residence
S
=
Scene of accident or acute event
X
=
Intermediate stop at physician's office on way to hospital (destination
code only)
Source: May 2009 Medicaid Update
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 32 of 52
Ambulance Services that have been approved to participate CMS Emergency Medical Triage,
Treat, and Transport (ET3) Model and in NYS Medicaid’s parallel model, may use the following
additional destination modifiers when appropriate.
W = Treated in Place
O = Physician’s Office
U = Urgent Care Facility
F = Federally Qualified Health Center
C = Community Mental Health Center (Includes Substance Use Treatment Centers)
No Additional Compensation for a Nursing Home-Provided Attendant
A number of nursing home administrators have inquired as to whether Medicaid residents or
their families may be charged a fee when a nursing home staff member accompanies a resident
to and from medical appointments outside the facility. For example: Nursing home personnel
travels with a resident to a medical appointment to provide necessary personal care services
and/or ensure effective communication between residents and medical practitioners. No
additional fee or compensation will occur in these scenarios and facilities cannot utilize an
elevated mode of transportation to accommodate facility staff.
3. Specific Minimum Qualifications by Category of Service
3.1 Ambulance Providers – Category of Service 0601
Only lawfully authorized ambulance services may receive reimbursement for the provision of
ambulance transportation rendered to Medicaid enrollees. An ambulance service must meet all
requirements of the NYSDOH. Ambulance services that are enrolled as NYS Medicaid
providers, but licensed to operate in a different state, must meet all requirements of their home
state.
Both non-emergency and emergency ambulance services are covered by the New York State
Medicaid program.
In non-emergency situations, a determination must be made by the appropriate prior
authorization official whether the use of an ambulance is medically necessary as opposed to a
non-specialized mode such as an ambulette, taxi/livery service, or public transportation.
A request for prior authorization for non-emergency ambulance transportation must be
supported by the Verification of Medicaid Transportation Abilities (Form 2015) of an ordering
practitioner who is the Medicaid enrollee's attending physician, physician assistant, or nurse
practitioner.
In cases of emergencies, emergency medical services are provided without regard to the
enrollee’s ability to pay, and no order or prior authorization is required. Payment will be made
only if transportation was actually provided to the enrollee. The only exception to this rule is for
treatment in place, provided by CMS and NYS Medicaid ET3-approved ambulance services.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 33 of 52
Ambulance services are granted operating authority by the NYSDOH. Ambulance services
whose operating authority has been revoked by the NYSDOH will be disenrolled from the
Medicaid program, thus precluding Medicaid payment.
Information regarding NYSDOH ambulance certification is located online at:
https://www.health.ny.gov/professionals/ems/
Rules for Requesting Non-Emergency Ambulance Transportation
A request for prior authorization for nonemergency ambulance transportation must be supported
by the documented order of a practitioner approved by the Department or prior authorization
official. All requests for ambulette and non-emergency ambulance transportation must include a
written form verifying MA transportation abilities as specified by NYSDOH.
A diagnostic and treatment clinic, hospital, nursing home, intermediate care facility, long term
home health care program, home and community-based services waiver program, or managed
care program may order non-emergency ambulance transportation services on behalf of the
ordering practitioner.
The ordering practitioner must document in the enrollee's patient record the condition which
necessitates the practitioner's ordering of a particular mode of transportation.
An ordering practitioner, or facilities and programs ordering transportation on the practitioner’s
behalf, which do not meet these rules, may be sanctioned according to the regulations
established by the NYSDOH.
National Provider Identifier
Ambulance providers must obtain and register a national provider identifier (NPI).
For emergency claims, ambulance providers must identify themselves as the service provider via
their NPI.
For non-emergency prior authorizations and claims, ambulance providers will be identified via
either their eight-digit Medicaid identification number or NPI.
An ambulance service may provide ambulette in addition to ambulance services; however, each
ambulance vehicle must meet staffing and equipment regulations of a certified ambulance at all
times, including occasions when an ambulance vehicle is used as an ambulette.
Territory
Ambulance services are certified to operate in an explicit primary geographic area, or territory.
Per Article 30 PHL §3010, every ambulance service certificate or statement of registration
issued under this article shall specify the primary territory within which the ambulance service
shall be permitted to operate. An ambulance service shall receive patients only within the
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 34 of 52
primary territory specified on its ambulance service certificate or statement of registration,
except:
(a) when receiving a patient which it initially transported to a facility or location outside its
primary territory;
(b) as required for the fulfillment of a mutual aid agreement authorized by the regional
council;
(c) upon express approval of the department and the appropriate regional emergency
medical services council for a maximum of sixty days if necessary to meet an emergency
need; provided that in order to continue such operation beyond the sixty day maximum
period necessary to meet an emergency need, the ambulance service must satisfy the
requirements of this article, regarding determination of public need and specification of the
primary territory on the ambulance service certificate or statement of registration; or
(d) an ambulance service or advanced life support first response service organization
formed to serve the need for the provision of emergency medical services in accordance
with the religious convictions of a religious denomination may serve such needs in an area
adjacent to such primary territory and, while responding to a call for such service, the
needs of other residents of such area at the emergency scene.
Nothing contained in this section shall be construed to prohibit any ambulance service
authorized by its governing authority to do so from transportation any sick or injured resident of
its primary territory from any general hospital or other health care facility licensed by the
Department, whether or not such general hospital or health care facility is within the service’s
primary territory, to any other general hospital or health care facility licensed by the Department
for further care, or to such resident’s homes.
In instances where no ambulance service possessing NYSDOH operating authority is able or
willing to accept a trip, the Broker will by necessity, and by the authority granted the Department
under the Mutual Assistance Plan of January 2, 2018, solicit assistance from an ambulance
service that does not currently have operating authority.
Questions regarding a company’s primary territory can be addressed by contacting the
NYSDOH Bureau of Emergency Medical Services at (518) 402-0996.
Source: February 2010 Ambulance Policy Reminder Letter
Basic Life Support (BLS) and Advanced Life Support (ALS)
In NYS, pre-Hospital care is delivered at either the basic life support (BLS) or advanced life
support (ALS) levels. At times, a basic life support ambulance may encounter a seriously ill or
injured patient who is in need of advanced life support care.
In these instances, the basic life support ambulance will often solicit assistance from either
another ambulance service, which is approved to provide advanced life support care, or from an
advanced life support first response service (ALSFR), which is a non-transporting entity that is
also authorized by the NYSDOH to provide ALS care.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 35 of 52
Only the transporting ambulance service may bill the Medicaid program (ALSFRs are
prohibited from enrolling as Medicaid providers).
Policy for Ambulance Services Cooperating with ALS Ambulance Services, or ALSRFs, to
Provide ALS Care:
BLS Ambulance services that have a cooperative arrangement with an ALSFR, or with an ALS
ambulance service shall, in the event of a cooperative emergency response where ALS services
are provided to the patient, be allowed to submit a claim for ALS and share the Medicaid
reimbursement with the ALSFR or ALS ambulance service.
As a precondition to reimbursement at the ALS fee, such ambulance services must:
1. Complete and submit to the Department the following form to effectuate affirmation of
contract/agreement in place between ALSFR, or ALS ambulance service, and the
transporting ambulance service to the Department.
2. Retain copies of any such contracts/agreements to be presented upon request to
Department officials.
3. Ensure that the ALSFR, or ALS ambulance service, maintains a copy of the same
agreement to be presented upon request of Department officials.
4. Ambulance services certified for basic life support only will submit claims for ALS service
when ALS service is rendered by the ALSFR, or ALS ambulance service, and reimburse
the ALSFR, or ALS ambulance service according to the contract/agreement.
5. Only ambulance services that have submitted affirmation of contract/agreement to the
Department will be allowed to submit a claim for ALS rendered by an ALSFR.
6. For auditing purposes, maintain complete records, including, but not limited to, claims,
contracts/agreements and the amount paid to the ALSFR, or ALS ambulance service.
Source: September 2010 Medicaid Update
Ambulance companies may not bill for both Basic Life Support (BLS) and Advanced Life
Support (ALS) services when ALS is provided. The provision of ALS services includes the
delivery of BLS services. Therefore, when an ambulance is sent to the scene of an emergency,
and personnel provide ALS transportation services, only the ALS service may be billed to the
Medicaid program.
Source: November 1999 Medicaid Update
ALS services must be provided by an advanced emergency medical technician. If an
ambulance company has not been properly certified to provide ALS services to patients, then the
company may not bill Medicaid for ALS services.
Questions regarding an ambulance services’ approved level of care can be addressed by the
NYSDOH Bureau of Emergency Medical Services staff at (518) 402-0996.
Specific Transportation Scenarios
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 36 of 52
Ambulance Transportation of Neonatal Infants to Regional Perinatal Centers
Ground ambulance transportation of critically ill neonates/newborns from community hospitals to
Regional Perinatal Centers (RPCs) is the responsibility of the RPC. Regionalization of neonatal
services into a single system of care was established by the Department to assure that each
infant who requires intensive care receives it as expeditiously as possible in the appropriate
facility. RPCs have affiliation agreements with community hospitals in their region.
The RPC will arrange for necessary ground ambulance services from the community hospital to
the RPC and the RPC is reimbursed directly by Medicaid for the costs of such transportation.
The RPC is responsible to find an RPC hospital bed and arrange for neonatal transportation of
the critically ill infant to the RPC.
At the time of discharge, the RPC will arrange for the transfer of the infant back to the
community hospital as needed. Upon discharge of the infant, transportation from the RPC back
to the community hospital is paid fee-for-service by Medicaid. Prior authorization of the transport
must be sought from the appropriate Prior Authorization Official.
Neither air transportation of neonatal infants nor maternal transportation is covered
under the regional Perinatal Center Program
Information regarding the RPC program is available at:
https://www.health.ny.gov/community/pregnancy/health_care/perinatal/regionalization_descrip.
htm
Source: August 2008 Medicaid Update
Transportation of a Hospital Inpatient
When a Medicaid enrollee is admitted to a hospital licensed under Article 28 of the Public Health
Law, the reimbursement paid to the hospital includes all necessary transportation services for
the inpatient.
If the admitting hospital sends an inpatient round trip to another hospital for the purposes of
obtaining a diagnostic test or therapeutic service, the original admitting hospital is responsible
for the provision of the transportation services. Therefore, the admitting hospital is responsible
to reimburse the ambulance (or other transportation) service for the transport of the inpatient.
For example, an admitting hospital arranges for the round trip of a Medicaid inpatient to another
hospital for a diagnostic test. The admitting hospital should reimburse the transportation provider
for the transport of the patient/enrollee.
Source: October 2006 Medicaid Update
Transportation from an Emergency Room to a Psychiatric Center
An ambulance may be requested to transfer a Medicaid enrollee undergoing an acute episode of
mental illness from an emergency room to a psychiatric hospital.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 37 of 52
For the safety of the patient, law enforcement, and hospital officials, when dealing with such a
person, must use an ambulance vehicle to transport that person to acute psychiatric care; not
non-emergency modes of transportation such as ambulette or taxi. The patient is in immediate
need of acute psychiatric care to be provided by such a facility. These ambulance transports are
considered emergency transports; therefore, prior authorization is not required and this should
be billed as a FFS emergency trip.
Transportation from an Emergency Room to a Trauma/Cardiac Care/Burn Center
An ambulance service may be requested to transfer a Medicaid enrollee from an emergency
room to a regional trauma, cardiac, or burn center. These ambulance transports are considered
emergency transports; therefore, prior authorization is not required and this should be billed as a
FFS emergency trip.
Transportation from an Emergency Room to an Emergency Room
At times, ambulance service may be requested to transport a Medicaid enrollee from an
emergency room to another emergency room. These ambulance transports are considered
emergency transports; therefore, prior authorization is not required and this should be billed as a
FFS emergency trip.
Transportation from an Emergency Room to Another Facility
Those urgent ambulance trips from an emergency department to another facility are also
considered by the Medicaid program an emergency and do not require prior authorization and
this should be billed as a FFS emergency trip.
Emergency Transport from One Hospital to Another Hospital, for a Higher Level of Care
Prior authorization is not required – do not contact the Transportation Broker
An ambulance may be requested to transfer a patient from one hospital to another hospital, in
emergency situations, when the patient requires specialized medical services that are not
available at the originating hospital. Examples of this include but are not limited to: transfers to
trauma, cardiac, burn, or stroke centers, or to another emergency room.
These ambulance transports are considered emergency transports; therefore, prior
authorization is not required.
Air Ambulance Guidelines and Reimbursement
In determining whether air ambulance transportation reimbursement will be authorized, the
following guidelines are used:
• The patient has a catastrophic, life-threatening illness or condition;

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 38 of 52
• The patient needs to be transported to a uniquely qualified hospital facility and ground
transport is not appropriate for the patient;
• Rapid transport is necessary to minimize risk of death or deterioration of the patient’s
condition; and
• Life-support equipment and advanced medical care is necessary during transport.
Fixed Wing Air Ambulance
The following fixed wing air ambulance services are reimbursable when the transport physically
occurs:
• Base fee;
• Patient loaded mileage;
• Physician (when ordered by hospital);
• Respiratory therapist (when ordered by the hospital, and only when the hospital is unable
to supply); and
• Destination ground ambulance charge (only when the destination is out of state).
The established fees assume the following:
• The provider will be responsible for advanced life support services, inclusive of all
services and necessary equipment, except as noted above.
• The provider will be responsible for paying the charges of ground ambulance at the
destination portion of the trip only when the destination is out-of-state. When the
destination is within New York State, the destination ground ambulance charge must be
billed to the Medicaid program by the ground ambulance provider that provided
transportation between the airport and hospital at the established basic life support fee.
• These amounts will be applied regardless of time or date of transport, i.e., day, night,
weekend and holiday.
• The provider will not seek nor accept additional reimbursement from the Medicaid enrollee
under any circumstance when billing the Medicaid program, other individuals or a facility,
except when a third-party insurance is billed, in which case the provider will be reimbursed
as follows:
o For patients covered by Medicare, Medicaid will pay the coinsurance and
deductible amount.
o For patients covered by other third-party insurances, Medicaid will pay the
coinsurance and deductible amount up to the established Medicaid
reimbursement fee. If the insurance company pays more than the established
Medicaid fee, Medicaid will not make any additional reimbursement.
o When an air ambulance bill is rejected by a third-party insurance with the
determination that the trip was medical unnecessary, the provider will not bill the
Medicaid program. If the third-party insurance pays at the ground ambulance fee,
Medicaid will reimburse as described above.
• The mileage fee will be applied only to patient loaded miles – those miles during which
the patient occupies the aircraft. Unloaded miles – those miles when the aircraft is in
transit to receive the patient or while the aircraft is returning to base – will not be charged.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 39 of 52
Helicopter (Rotary Wing) Air Ambulance
The following helicopter air ambulance services are reimbursable:
• Base fee
• Patient occupied flight mileage
Insurance Clarifications
Submitting a Claim Deemed by the Primary Insurer to be Non-Emergency
When submitting a claim to the Medicaid program for a transport deemed by Medicaid to be
emergency pursuant to the policies stated in this Manual, but to be non-emergency by the
enrollee's primary insurer, the ambulance vendor submits a claim to Medicaid using the
applicable procedure code (i.e., that code used to bill the primary insurer) with the emergency
indicator checked. Please read and review the billing manuals on the eMedNY website:
https://www.emedny.org/ProviderManuals/Transportation/index.aspx
Additionally, the claimant must properly complete the third-party payment fields on the claim.
Subrogation Notice
When a Medicaid enrollee has both commercial insurance in which the ambulance company is
not a participating provider, and has active Medicaid coverage, the ambulance company can
send a “Medicaid Subrogation Notice” to the commercial insurance company advising them to
pay the ambulance provider as an agent of the NYSDOH.
Note: Providers not participating in Medicare cannot bill Medicare regardless of the New
York State Subrogation Laws.
The Medicaid Subrogation Notice can be obtained from the local department of social services.
Source: April 2008 Medicaid Update
Medicare Involvement
Medicare, in many instances, is obligated to pay for ambulance transportation for patients with
Medicare Part B coverage. Medicare guidelines require that the patient be suffering from an
illness or injury which contraindicates transportation by any other means. This requirement is
presumed to be met when the patient:
• Was transported in an emergency situation (e.g., as a result of an accident, injury or acute
illness);
• Needed to be restrained;
• Was unconscious or in shock;

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 40 of 52
• Required administration of oxygen or other emergency treatment on the way to the
destination;
• Had to remain immobile due to a fracture that had not been set, or the possibility of a
fracture;
• Sustained an acute stroke or myocardial infarction;
• Was experiencing severe hemorrhage;
• Was bed-confined before and after the ambulance trip; or
• Could be moved only by stretcher.
Ambulance services shall submit a claim to the Medicare Administrative Contractor (MAC) when
transportation has been provided to a Medicare eligible person. Upon approval by Medicare of
the claim, a claim may be submitted to Medicaid for cross-over payment. Claims for ambulance
services will be reviewed by the Medicaid program to determine if the Medicaid enrollee has
Medicare and if the provider billed Medicare prior submission of the claim to Medicaid.
When an ambulance service has been instructed by the Medicare carrier not to submit a claim
to the carrier for the ambulance transportation of a person covered under Medicare Part B
because Medicare does not cover that particular service (e.g., the transport of a person to a
physician’s office), the ambulance service must submit evidence of such instructions to the Prior
Authorization Official. The Prior Authorization Official will then determine if Medicaid
reimbursement will be authorized.
Ambulance services are covered under Medicare Part A when a hospital inpatient is transported,
round-trip, to and from another hospital or freestanding facility to receive specialized treatment
not available at the first hospital. The ambulance service is included in the hospital’s Medicare
Part A payment. In such situations when an ambulance service transports a hospital inpatient
covered under Medicare to medical care not available at the hospital, the ambulance service
shall seek reimbursement from the hospital. The provider shall not seek authorization from the
Prior Authorization Official nor shall the provider submit a claim for Medicaid for reimbursement.
Generally, when an original admitting hospital sends a Medicaid inpatient to another hospital,
round-trip, for the purposes of obtaining a diagnostic or therapeutic service not available in the
admitting hospital, the original hospital is responsible for the costs of transportation. Neither
hospital may bill the Medicaid program separately for the transportation services. The hospital
should reimburse the ambulance or other transportation service for the transport of the patient,
as the Medicaid inpatient fee is inclusive of all services provided to the patient. The transport
will not be authorized by the Prior Authorization Official, nor paid fee-for-service.
When a patient covered under Medicare is discharged from one hospital and is transported from
that hospital to a second hospital for purposes of admission as an inpatient to the second
hospital, the ambulance service is paid for under Medicare Part B. The provider shall submit a
claim to the Medicare Administrative Contractor (MAC).
Medicaid will not reimburse claims that are not approved by Medicare or other insurance when a
determination has been made that transportation by ambulance was not medically necessary.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 41 of 52
Regulation 18 NYCRR §360-7.3, applicable to this policy, can be found online at:
http://www.health.ny.gov/regulations/nycrr/title_18/.
Medicare Denied “Excess Mileage”
Medicare will reimburse ambulance providers mileage to the closest appropriate hospital. If the
ambulance travels to a more distant hospital, only the mileage to the closest hospital is covered;
any additional mileage is not covered by Medicare. Appropriate is defined as a hospital capable
of caring for the patient in their current medical condition.
For example, the enrollee was in Cortland County when his pacemaker began to fail. His
cardiologist, who installed the pacemaker, is in Syracuse, and wanted to see the patient at St.
Francis Hospital (Syracuse) as soon as possible. Medicare only paid for the miles to the nearest
hospital in Cortland (presuming that the hospital in Cortland is able to care for a patient with a
failing pacemaker), leaving the ambulance provider thirty-three (33) unreimbursed miles.
Below is Medicaid’s policy regarding the 33 miles left unreimbursed by Medicare:
When an ambulance service delivers a transport of a Medicaid enrollee who is
also covered under Medicare, the ambulance provider must bill Medicare, and
then Medicaid will pay the coinsurance and deductible amounts on the
approved Medicare claim.
This issue of unreimbursed miles is an issue between the ambulance provider
and Medicare; Medicaid will not authorize reimbursement for extra miles denied
by Medicare. These miles are a Medicare-covered service, Medicare has
considered them for payment, and adjudicated the claim.
Payment under the fee schedule for ambulance services:
• Includes a base fee payment plus a payment for mileage;
• Covers both the transport of the enrollee to the nearest appropriate facility and all items
and services associated with such transport; and
• Precludes a separate payment for items and services furnished under the ambulance
benefit.
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c15.pdf
3.2 Ambulette Providers – Category of Service 0602
Only lawfully authorized ambulette services may receive reimbursement for the provision of
ambulette transportation. Ambulettes must comply with all NYS Department of Transportation
(NYSDOT) licensure, inspection and operational requirements, including those identified at Title
17 NYCRR §720.3(A).

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 42 of 52
Ambulette drivers must be qualified under Article 19A of the New York State Department of
Motor Vehicles’ Vehicle and Traffic Law.
Ambulette as Taxi/Livery
An ambulette may provide taxi (curb-to-curb) service as long as the ambulette maintains the
proper authority and license(s) to operate as an ambulette. The Medicaid program does not
require the ambulette to be separately licensed as a taxi/livery service; rather, it operates as an
ambulette providing taxi/livery service. In these situations, the ambulette will be assigned the
taxi level procedure codes required for billing.
Where applicable, proof of licensure by the local Taxi and Limousine Commission is required as
a condition of enrollment. In such instances, compliance with local Taxi and Limousine
Commission regulations is required.
Potential new vendors should contact the prior authorization official in the area(s) in which they
intend to operate to inquire about local certification requirements.
New York City Taxi & Limousine Licensure Requirement for Ambulette Companies
Having Contract Carrier Permits Issued by the New York State Department of
Transportation
Effective January 28, 2016, the Department no longer requires that New York City ambulette
providers who have been granted contract carrier permits by the New York State Department of
Transportation (NYSDOT) be licensed by the New York City Taxi and Limousine Commission
(NYCTLC).
Ambulettes vehicles are regulated by NYSDOT. The NYSDOH recognizes that some ambulette
providers added sedans and minivans to their fleets in order to transport ambulatory patients in
need of curb-to-curb transportation billable to the Medicaid program under livery procedure
codes. NYSDOT will not inspect these sedans and mini vans. Consistent with current practices
of the NYSDOT, only Medicaid transports performed by ambulette providers in ambulette
vehicles, must be performed in vehicles inspected semi-annually by the NYSDOT and by drivers
certified under Article 19A of Vehicle and Traffic Law. Accordingly, ambulette providers may
continue to use sedans and minivans to provide livery transports.
Medicaid reimbursement is available to lawfully authorized ambulette providers for ambulette
transportation furnished to Medicaid enrollees whenever necessary to obtain medical care.
Transportation services are limited to the provision of passenger-occupied transportation to or
from Medicaid-covered services. The Prior Authorization Official must make a determination
whether the use of an ambulette, rather than a non-specialized mode of transportation such as
taxi or public transportation, is medically necessary. An ambulette may not be used as an
ambulance to provide emergency medical services.
Ambulette services are bound by the operating authority granted them by the NYSDOT. In
accordance with NYSDOT procedures, each service is given the authority to operate within a
specific geographic area. In that specified area, unless contraindicated by the ambulette
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 43 of 52
services’ NYSDOT-issued license, transportation is to be “open to the public” and is not to be
withheld between any points within the boundaries of the service’s operating authority when the
ambulette service is open for business. Thus, an ambulette service participating in the Medicaid
program at the current Medicaid reimbursement fee may not refuse to provide Medicaid
transportation within the ambulette service’s area of operation, as this constitutes a violation of
New York State Transportation Law §146 which reads
“…It shall be the duty of every motor carrier to provide adequate service,
equipment and facilities under such rules and regulations as the
Commissioner may prescribe.”
Ambulette services found guilty of violating New York State Transportation laws may face fines
and possible revocation of operating authority, as determined by NYSDOT. Those ambulette
services whose operating authority has been revoked by the NYSDOT will be disenrolled from
the Medicaid program, thus precluding Medicaid payment.
Source: March 2011 Medicaid Update
Stretcher Ambulette
Stretcher service is considered non-emergency transportation of a Medicaid enrollee who must
be transported to and from medical care, is confined to bed, cannot sit in a wheelchair, and
does not require medical attention/monitoring during transport.
A stretcher service can transport a person who self-administers oxygen. The employee of the
stretcher service is not permitted to assist with the supply oxygen at any time to an enrollee.
Further, at no time shall the transportation provider and his/her employees offer oxygen to a
passenger, nor shall a stretcher ambulette be equipped with oxygen or oxygen delivery
supplies.
A stretcher service shall not transport an enrollee who requires medical attention/monitoring or
any type of medical treatment.
A stretcher service shall not transport an enrollee who is medically sedated.
The stretcher service requires at least two (2) employees to transport the enrollee. At all times,
the stretcher service must supply the needed personnel to safely lift and transport a Medicaid
enrollee.
The stretcher service is expected to move the stretcher over impediments such as curbs and
doorways, and up and down steps where an elevator or ramp is unavailable. Necessary
personnel, and/or supplemental equipment, must be available to overcome such impediments.
Requirements for Participation as a Stretcher Service
To participate in the New York State Medicaid program, a provider must meet all applicable
State, County and Municipal requirements for legal operation; as well as the quality
performance indicators listed in this Manual.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 44 of 52
The Broker may require certification from stretcher transportation vendors that the expectations
listed in this manual are met or exceeded .
Equipment/Safety Requirements for Stretcher Service
Every stretcher ambulette shall be equipped with a wheeled stretcher (cot), which must be used
strictly in accordance with the manufacturer’s instructions
Every stretcher ambulette shall be equipped with the stretcher (cot) manufacturer’s supplied
patient restraint straps, which must be used strictly in accordance with the manufacturer’s
instructions.
Every stretcher ambulette shall be equipped with a stretcher (cot) retention device, which must:
1. Be securely attached to the vehicle in accordance with the manufacturer’s instructions.
2. Be compatible with the vehicle’s stretcher (cot) and be manufactured by the same entity
as the stretcher.
3. Be used strictly in accordance with the manufacturer’s instructions, at all times.
Oxygen tanks must be secured while in the vehicle.
Stretcher Vehicle Requirements
A. Each vehicle shall comply with applicable requirements of the NYSDOT, the NYCTLC
(when operating in New York City), or any other local agency that regulates the operation
of a stretcher carrying vehicle.
B. Each vehicle shall be staffed with at least a driver and one (1) assistant, commensurate
with the needs of the individual being transported, and shall only be used to transport an
individual who needs transportation to or from a non-emergency medical appointment or
service, is convalescent or otherwise non-ambulatory and cannot use a wheelchair, and
who does not require medical monitoring, medical aid, medical care or medical treatment
during transport.
C. The assistant shall be seated in the passenger compartment while the vehicle is
transporting a patient and shall notify the driver immediately of any sudden perceived
change in the individual’s condition.
Ambulettes and “Star of Life” Logo
The "Star of Life" logo is to be used to identify emergency response vehicles that
respond to an emergency situation that may necessitate medical care.
It is inappropriate for this symbol to be affixed to a vehicle operated by a non-
medical provider.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 45 of 52
The Star of Life is a registered ® image owned by the National Highway Safety Administration’s
Office of EMS https://www.ems.gov/staroflife.html
Source: November 2009 Medicaid Update
Rules for Requesting Ambulette Transportation
Per 18 NYCRR Section 505.10(d)(8) a request for prior authorization for transportation by
ambulette or paratransit vehicle must be supported by the written order of an ordering
practitioner who is the Medicaid enrollee's attending physician, physician assistant, nurse
practitioner, dentist, optometrist, podiatrist or other type of medical practitioner approved by the
department. All requests for ambulette and non-emergency ambulance transportation must
include a written form verifying MA transportation abilities as specified by the department.
A diagnostic and treatment clinic, hospital, nursing home, intermediate care facility, long term
home health care program, home and community based services waiver program, or managed
care program may order non-emergency ambulance transportation services on behalf of the
ordering practitioner.
Note: The ordering practitioner must note in the patient’s medical record the Medicaid
enrollee’s condition which qualifies use of ambulette transportation.
The ordering practitioner must document in the enrollee's patient record the condition which
necessitates the practitioner's ordering of a particular mode of transportation.
Any ordering practitioner or entity ordering transportation on the practitioner’s behalf that orders
transportation which is deemed not to meet the above rules may be sanctioned according to 18
NYCRR §515.3.
Enrollee Assistance
Personal Assistance, Escorts and Carry-Downs
Personal assistance by the staff of the transportation company is required by the Medicaid
program and consists of the rendering of physical assistance to the ambulatory and non-
ambulatory (wheelchair-bound) Medicaid enrollees in:
• Walking, climbing or descending stairs, ramps, curbs, or other obstacles;
• Opening and closing doors;
• Accessing an ambulette vehicle; and
• The moving of obstacles as necessary to assure the safe movement of the Medicaid
enrollee.
There is no separate reimbursement for the escort of a Medicaid enrollee. Necessary escorts
are to be provided by the ambulette service at no additional or enhanced charge.
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 46 of 52
The Medicaid program does not limit the number of stairs or floors in a building that a
provider must climb in order to deliver personal assistance to a Medicaid enrollee. The
ambulette provider is required to provide personal assistance and door-to-door service at no
additional or enhanced charge. This means the staff must transport the enrollee from his/her
front door (including apartment door, nursing home room, etc.) no matter where it is located; to
the door of the medical practitioner from whom the enrollee is to receive Medicaid-covered
medical services.
Please note that the Office of the Medicaid Inspector General (OMIG) has conducted
preliminary on-site field reviews of various ambulette services and found that many service
providers did not provide personal assistance as required. If, upon audit, the OMIG finds
personal assistance was not provided by the ambulette service provider, the provider who billed
for ambulette service may be subject to financial or other provider-specific sanctions, as
designated by the OMIG.
Source: September 2002 Medicaid Update ; August 2011 Medicaid Update
Transporting a Medicaid Enrollee Who Needs to be Lifted onto an Examination Table
Medicaid will reimburse for the most appropriate mode of transportation required to transport an
eligible enrollee to a Medicaid-covered service. Due to the increasing number of wheelchair
users with excessive weight issues and other disabilities that are unable to transfer out of a
wheelchair, the enrollees are faced with the prospect of requiring a lift out of the wheelchair onto
an examination table.
When a wheelchair user is unable to move from the wheelchair and needs to be lifted (i.e.,
transferred) from the wheelchair onto an examination table, this transfer is the responsibility of a
personal aide of the enrollee and/or medical practitioner. Lifting of the enrollee is not the
responsibility of the transportation driver.
It is not appropriate to request the stretcher mode of transportation for an enrollee in
order for the enrollee to be transferred easily onto the examination table by the stretcher
personnel. Stretcher mode is inappropriate for transportation purposes when the
enrollee can be safely transported in a wheelchair.
For wheelchair users who need assistance in getting out of their chair, providers who order
transportation need to coordinate the enrollee’s medical care among those practitioners who are
able to accommodate the lifting of the enrollee onto the examination table.
Transportation vendors shall not be required to:
• accompany the enrollee throughout their appointment for the purposes of relaying
treatment information to the nursing home staff or caregiver;
• enter an examination room for the purposes of transferring the enrollee on or off of an
examination table; nor,
• leave provider-owned equipment (i.e., a stretcher) at the treating facility in order for the
medical practitioner to render necessary treatment.
Source: December 2011 Medicaid Update

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 47 of 52
Surety Bond Requirement
The OMIG has found that several ambulette providers have gone out of business or changed
ownership while having outstanding debts owed to the Medicaid program. Medicaid regulations
allow for financial security, provided in the form of surety bonds, to be required as a condition of
participation or continued enrollment in the Medicaid program for providers where claims
submitted for payment are expected to exceed $500,000 in a single year or $42,000 in any
month.
The OMIG has determined that applicants for ambulette services located in Nassau,
Westchester, Monroe, Erie, Orange and Suffolk Counties that submit their applications on or
after March 1, 2011, will be required to submit a surety bond prior to enrollment if the ambulette
provider is determined to be otherwise eligible for enrollment.
In New York City, ambulette providers enrolled as a result of an ownership change will be
required to submit a bond.
The surety bond requirement will apply to all applicants for new enrollment in the Medicaid
program with service addresses in the counties listed above, and for enrollment as a result of an
ownership change in New York City and the counties listed above where there is a new entity
purchasing the company. The initial bond must be submitted prior to enrollment and the term of
the bond must be for at least one calendar year.
The applicant will be contacted by the OMIG once an initial determination has been made that
enrollment can otherwise be granted. At that time, the provider will be asked to submit a surety
bond within 90 days in order to secure enrollment. If an applicant fails to provide a bond, the
application will be denied.
The OMIG will request surety bonds for ambulette providers in the amount of $100,000 per year
per applicant, or $25,000 per year for each ambulette owned or used by the applicant,
whichever amount is lower. All surety bonds must be renewed annually. If the amount initially
requested is less than $100,000, the amount of the bond may increase, up to $100,000, upon
renewal if the number of ambulettes owned or used by the applicant increases. It should be
noted that surety bonds are issued by insurance companies and the amount of the bond would
be much higher than the actual cost to the applicant.
If an applicant estimates that the company will bill less than $500,000 for ambulette services in
the first full year of Medicaid enrollment, the applicant may submit a letter with the company’s
enrollment application stating this and requesting an exception to the bond requirement. The
letter must include an estimate of the company's annual Medicaid billings, as well as the
number of ambulettes the company owns or leases and plans to purchase or lease in the first
year of operation. OMIG will review this information, as well as billings of similar companies, to
make a determination as to whether the bond will be required.
In addition to the pre-enrollment bond requirement in the counties listed above, all applicants
approved for enrollment for ambulette services that submit an application on or after March 1,
2011, regardless of where the company is located, will be subject to a review of claims after

Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 48 of 52
enrollment to determine if Medicaid billings exceed $500,000 per year or $42,000 in any month. If
billings exceed that threshold, a surety bond for $100,000 per year (or $25,000 per year for
each ambulette owned or used by the applicant during the period reviewed if that amount is
lower), will be required for continued enrollment. Failure to provide a bond within 90 days will
result in termination from the Medicaid program.
All surety bonds must be renewed annually while the provider is enrolled in the Medicaid
program. The provider will be given notice that renewal is required at least sixty days prior to the
expiration date. Failure to renew a bond by the expiration date will result in termination
from the Medicaid program. If a provider's billings have dropped below the required threshold
of $500,000 per year for the year that the surety bond was in effect, the provider may submit a
request to be relieved of the obligation to provide a bond at the time renewal is required by
Medicaid.
Source: March 2011 Medicaid Update
3.3 Taxi (Category of Service 0603) and NYC Livery (Category of Service 0605) Providers
To participate in the Medicaid program, a taxi/livery provider must meet all applicable State,
County, and Municipal requirements for legal operation (including local Taxi and Limousine
Commission licensure, where applicable).
All taxi and livery providers transporting Medicaid enrollees must adhere to all local municipal
and regulatory agency license plate requirements. This level of service is curb to curb and
personal assistance (door through door) is not required.
Rules for Requesting New York City Livery Transportation
A request for transportation via New York City livery service must be supported by the order of a
practitioner who is the Medicaid enrollee’s medical provider.
Prior authorization of taxi and livery services is required to ensure that a Medicaid enrollee uses
the means of transportation most appropriate to his medical needs. Requests for taxi/livery
services shall be made in advance by either the enrollee or the enrollee’s medical provider.
It is critical that, before a transport is provided to a Medicaid enrollee, the transportation provider
verify the person’s eligibility for Medicaid on the date of service. Reimbursement will not be
made for services rendered to persons ineligible for Medicaid-funded transportation.
3.4 Transportation Network Companies (TNC) - Category of Service 0609 Providers
To participate in the Medicaid program, a TNC/high-volume-for-hire-service provider must meet
all applicable State, County, and Municipal requirements for legal operation (including New York
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 49 of 52
State Department of Motor Vehicle Transportation Network Company and Limousine
Commission licensure, where applicable).
Prior authorization of TNC/high-volume-for-hire-services is required to ensure that a Medicaid
enrollee uses the means of transportation most appropriate to his medical needs. Requests for
this level of service shall be made in advance by either the enrollee or the enrollee’s medical
provider.
Information regarding the submission of claims is available in the Billing Guidelines Manual at:
http://www.emedny.org/ProviderManuals/Transportation/index.html.
Upon request, the Medicaid eMedNY Contractor provides on-site billing training. To schedule
such training, please call (800) 343-9000.
4. Document Control Properties
Control Item
Value
Document Name
Medicaid Transportation Policy Manual
Document Control Number
2023-1
Document Type
Policy Manual
Document Version
2023-V1
Document Status
Final
Effective date
August 25, 2023
Appendix 1 – Ambulance Service and Advanced Life Support Form
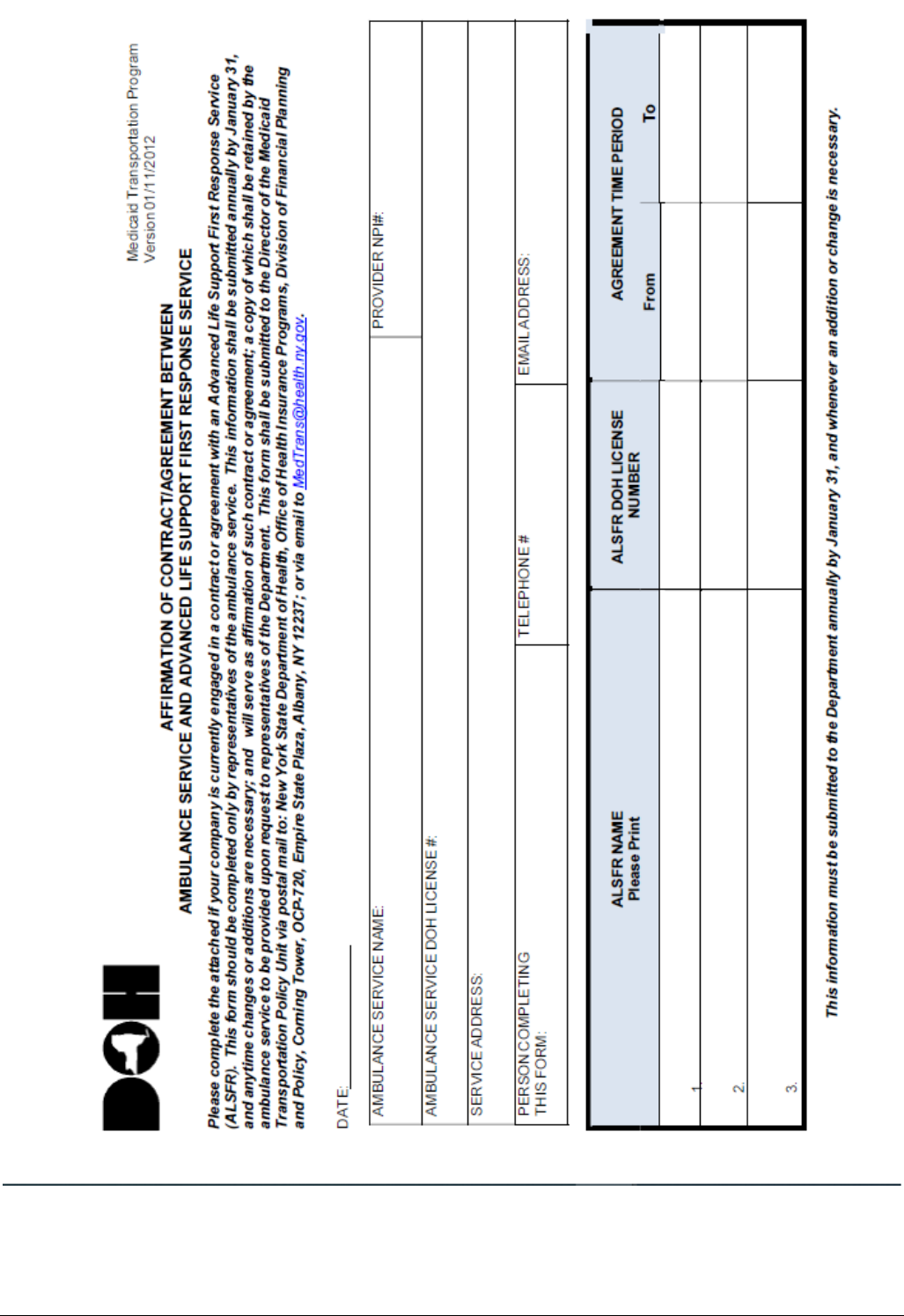
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 50 of 52
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 51 of 52
Appendix 2 – Acceptable Claim Modifiers
Acceptable Claim Modifiers
DIAG THERA SITE NOT P OR H ORIG/RES, DOM, CUST FACIL
DE
DIAG THERA SITE NOT P OR H ORIG/HOSP BASE DIALYSIS
DG
DIAG THERA SITE NOT P OR H ORIG/HOSPITAL
DH
DIAG THERA SITE NOT P OR H ORIG/TRANS BETW AMB MOD
DI
DIAG THERA SITE NOT P OR H ORIG/NON-HOSP DIALYSIS
DJ
DIAG THERA SITE NOT P OR H ORIGIN CODES/SNF
DN
DIAG THERA SITE NOT P OR H ORIGIN CDS/PHYS OFFICE
DP
DIAG THERA SITE NOT P OR H CDS/RESIDENCE
DR
DIAG THERA SITE NOT P OR H ORIG/DEST INTERM STOP
DX
RES, DOM, CUST FAC (NOT1819)/DIAG THERA NOT P OR H
ED
RES, DOM, CUST FAC (NOT1819)/HOSP BASE DIALYSIS
EG
RES, DOM, CUST FACILTY(NOT 1819)/HOSPITAL
EH
RES, DOM, CUST FAC /SITE TRANS BETWEEN AMBUL MODES
EI
RES, DOM, CUST FAC(NOT 1819)/ NON- HOSP DIALYSIS
EJ
RES, DOM, CUST FAC(NOT 1819)/ SNF 1819 FACILITY
EN
RES, DOM, CUST FAC(NOT 1819)/ RESIDENCE
ER
RES,DOM,CUST FAC(NOT 1819)/DEST CD INTR STP
EX
HOSP DIALYSIS FAC/ORIG DIAG THER SITE NOT P OR H
GD
HOSP DIALYSIS FAC/RES, DOM, CUST FAC (NOT 1819)
GE
HOSP DIALYSIS FACILITY (HOSP RELATED)/ HOSPITAL
GH
HOSP DIALYSIS FAC/SITE OR TRANS BETW AMBUL MODES
GI
MULTIPLE PATIENT TRANSPORT
GM
HOSP DIALYSIS FAC(HOSP RELATED)/SNF (1819 FAC)
GN
HOSP DIALYSIS FAC(HOSP RELATED)/PHYSICIANS OFFICE
GP
HOSP DIALYSIS FAC(HOSP
GR
HOSPITAL/HOSP DIALYSIS FACILITY(HOSP OR HOSP RELAT)
HG
HOSPITAL/HOSPITAL
HH
HOSPITAL/SITE OF TRANS BETW MODES OF AMBUL TRANSP
HI
HOSPITAL/NON-HOSPITAL BASED DIALYSIS FACILITY
HJ
HOSPITAL/SKILLED NURSING FACILITY SNF (1819 FAC)
HN
HOSPITAL/PHYSICIAN'S OFFICE
HP
HOSPITAL/RESIDENCE
HR
HOSPITAL/DEST CD INTERM STOP AT PHYS OFC TO HOSP
HX
SITE OF TRAN BETW MODE OF AMB/DIAG THER NOT P OR H
ID
SITE OF TRANS BETW MODE OF AMB/HOSP BASED DIALYSIS
IG
SITE OF TRANS BETWEEN MODES OF AMBULANCE/HOSPITAL
IH
SITE OF TRANS BETWEEN TYPES OF AMBULANCE to SITE OF TRANSFER
II
SITE OF TRANS BETW MODES OF AMB/NON-HOSP DIALYSIS
IJ
SITE OF TRANS BETW MODES OF AMB/SNF (1819 FACILITY)
IN
SITE OF TRANS BETW MODES OF AMB TRANS/PHYS OFFICE
IP
SITE OF TRANS BETW MODES OF AMB/DEST INTERM STOP
IX
NON-HOSP DIALYSIS FAC/DIAG THERA ORIGIN NOT P OR H
JD
NON-HOSP DIALYSIS FAC/RES, DOM, CUS FAC (NOT 1819)
JE
NON-HOSPITAL BASED DIALYSIS FACILITY/HOSPITAL
JH
NON-HOSP DIALYSIS FAC/SITE OF TRANS BETW MODES AMB
JI
NON-HOSP BASED DIALYSIS FAC/SNF (1819 FACILITY)
JN
NON-HSP-BASED DIALYSIS FACILITY/PHYS OFC
JP
NON-HOSPITAL BASED DIALYSIS FACILITY/RESIDENCE
JR
NON-HOSP DIALYSIS FAC/DEST CD INTERM STOP AT PHYS
JX
SNF (1819 FACILITY)/DIAG THERA ORIGIN(NOT P OR H)
ND
SNF (1819 FACILITY)/HOSP BASED DIALYSIS(HOSP RELAT
NG
SNF (1819 FACILITY)/HOSPITAL
NH
SNF (1819 FACILITY)/TRANS BETWEEN MODES OF AMBUL
NI
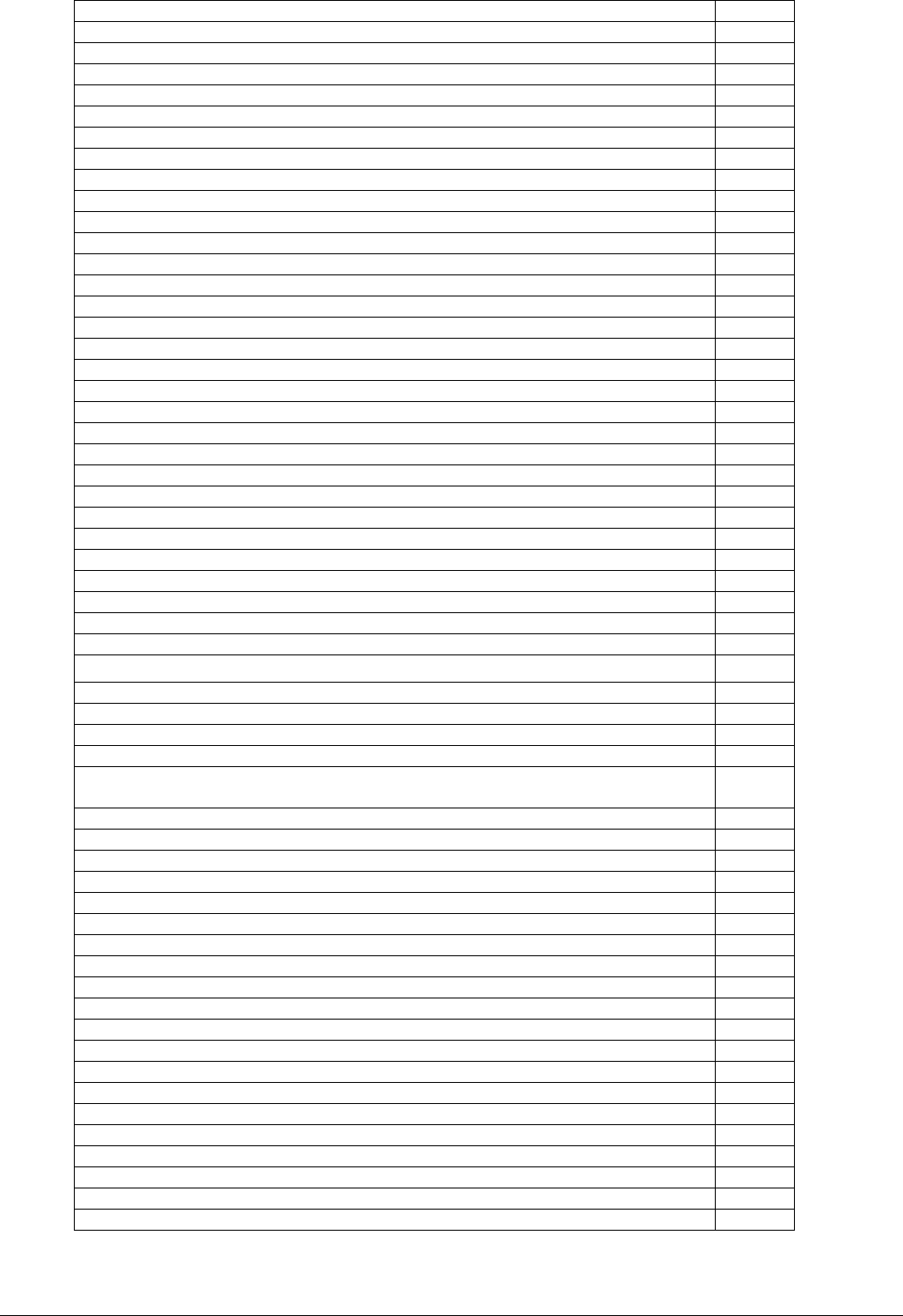
Medicaid Transportation Policy manual Effective Date: 08/25/2023
Page 52 of 52
SNF (1819 FACILITY)/NON-HOSP BASED DIALYSIS FACIL
NJ
SNF (1819 FACILITY)/SNF (1819 FACILITY)
NN
SNF (1819 FACILITY)/PHYSICIAN'S OFFICE
NP
SNF (1819 FACILITY)/RESIDENCE
NR
SNF (1819 FACILITY)/DEST CD INTERM STOP PHYS OFFIC
NX
PHYS OFFICE/DIAG THERA SITE ORIGIN CDS NOT P OR H
PD
PHYS OFFICE/RES, DOM, CUS FACILITY(NOT 1819 FACIL)
PE
PHYS OFFICE/HOSP BASED DIALYSIS FACILITY
PG
PHYSICIAN'S OFFICE/HOSPITAL
PH
PHYS OFC/SITE OF TRANS BETWE MODES OF AMBUL TRANSP
PI
PHYS OFFICE/NON-HOSPITAL BASED DIALYSIS FACILITY
PJ
PHYSICIAN'S OFFICE/SNF (1819 FACILITY)
PN
PHYSICIAN'S OFFICE/RESIDENCE
PR
PATIENT PRNCD DEAD AFTER AMBLNCE
QL
AMBULANCE SERVICES UNDER ARRANGEMENT BY A HOSPITAL
QM
AMBULANCE SERVICES FURNISHED DIRECTLY BY A HOSPITAL
QN
RESIDENCE/DIAG THERA SITE ORIGIN CDS NOT P OR H
RD
RESIDENCE/HOSPITAL BASED DIALYSIS FACILITY
RG
RESIDENCE/HOSPITAL
RH
RESIDENCE/SITE OF TRANS BETWE MODES OF AMBUL TRANS
RI
RESIDENCE/NON-HOSPITAL BASED DIALYSIS FACILITY
RJ
RESIDENCE/SKILLED NURSINC FACILITY (SNF)(1819 FAC)
RN
RESIDENCE/PHYSICIAN'S OFFICE
RP
RESIDENCE/DEST CD INTERM STOP AT PHYS OFF TO HOSP
RX
SCENE OF ACCIDENT ACUTE/DIAG THER ORIG NOT P OR H
SD
SCENE OF ACCIDENT ACUTE EVENT/HOSP BASED DIALYSIS
SG
SCENE OF ACCIDENT ACUTE EVENT/HOSPITAL
SH
SCENE OF ACCIDENT ACUTE/TRANS BETW MODES AMBUL TRA
SI
SCENE OF ACCIDENT OR ACUTE/NON- HOSP BASED DIALYSIS
SJ
SCENE OF ACCIDENT OR ACUTE EVENT/SNF (1819 FAC)
SN
SCENE OF ACCIDENT OR ACUTE EVENT/PHYSICIAN'S OFFIC
SP
DEST CD INTERM STOP AT PHYS OFC ON WAY TO HOSP
SX
Residential, Domiciliary, Custodial Facility Other Than SNF/Treat in Place
EW
Residential, Domiciliary, Custodial Facility Other Than SNF/Physician’s Office
EO
Residential, Domiciliary, Custodial Facility Other Than SNF/Urgent Care Facility
EU
Residential, Domiciliary, Custodial Facility Other Than SNF/FQHC
EF
Residential, Domiciliary, Custodial Facility Other Than SNF/Community Mental
Health/SUD
EC
SNF/Treat in Place
NW
SNF/Physician’s Office
NO
SNF/Urgent Care Facility
NU
SNF/FQHC
NF
SNF/Community Mental Health/SUD
NC
Physician’s Office/Treat in Place
PW
Physician’s Office/Physician’s Office
PO
Physician’s Office/Urgent Care Facility
PU
Physician’s Office/FQHC
PF
Physician’s Office/Community Mental Health/SUD
PC
Residence/Treat in Place
RW
Residence/Physician’s Office
RO
Residence/Urgent Care Facility
RU
Residence/FQHC
RF
Residence/Community Mental Health/SUD
RC
Scene of Accident or Acute Event/Treat in Place
SW
Scene of Accident or Acute Event/Physician’s Office
SO
Scene of Accident or Acute Event/Urgent Care Facility
SU
Scene of Accident or Acute Event/FQHC
SF
Scene of Accident or Acute Event/ Community Mental Health/SUD
SC
